|

Custom Search
|
|
Infectious Disease Online Pathology of Actinomycosis
|
|
Actinomycosis is
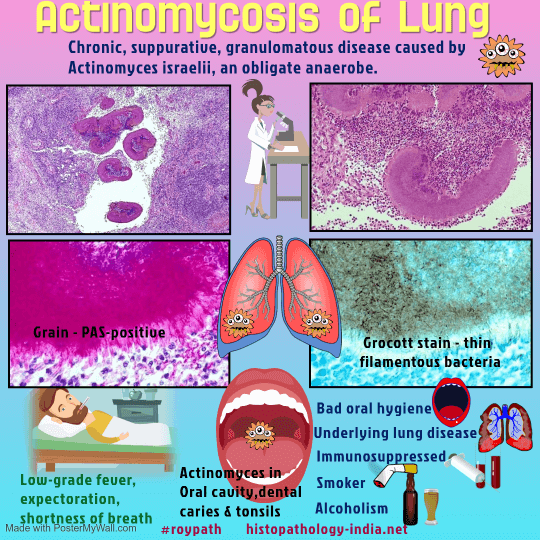
a chronic suppurative disease caused by anaerobic filamentous bacteria
in the order Actinomycetales.
The disease occurs worldwide and is mostly seen in tropical regions such as Asia, Africa, central and south America. Males are more frequently affected. The principal agent of actinomycosis in humans is Actinomyces israelii - a gram-positive, branching, anaerobic or microaerophilic bacterium. This organism occur as commensals in the mouth and "sulphur" granules are commonly found in the tonsillar crypts of healthy persons. The actinomycetes are ordinarily of low pathogenicity. Underlying disease and interruption of mucocutaneous barriers predispose a person to actinomycosis by providing a medium in which these endogenous organisms can invade, proliferate and disseminate. Unlike nocardiosis, actinomycosis does not occur preferentially in patients with defective immunity.
Note: The diagnosis of actinomycosis, especially in the extremity, must be separated from actinomycetoma and botryomycosis. Botryomycosis is a chronic bacterial infection of soft tissues that produces loose clumps of bacteria resembling granules. It is easily separated from actinomycosis by the presence of cocci or nonbranching bacilli. Actinomycetoma is a form of madura foot or mycetoma and caused by nocardia species. Actinomycosis of an extremity and actinomycetoma can produce virtually the same disease characteristics (localized chronic and progressive infection with purulent sinus tract drainage containing granules and involvement of contiguous bone).
In Actinomycosis patients present with painless swelling of foot and is usually not associated with fever. The organism produce chronic destructive lesions of deep soft tissue and bones, most commonly of the limbs. Infection commonly occurs in the foot of bare-footed persons. Primary skin infections may develop after human bites.
Based on the anatomic site of lesions four clinical forms of actinomycosis are recognized: (i) Cervicofacial - Most commonly involved is the cervicofacial area, where the disease is often a sequel to dental caries, periodontal disease, or injury to the oral mucosa, such as tooth extraction. The localized lesion enlarges, abscesses form, and draining sinus tracts which ruptures with formation of sinuses through which "sulfur grains" are discharged. If untreated, the infection may extend into the mandible, paranasal sinuses, orbit, cranial bones, and thorax, where it may then disseminate to the central nervous system, skin, and other bones. (ii) Thoracic - Infection occurs due to aspiration of infective material. (iii) Abdominal - Abdominal actinomycosis is frequently mistaken clinically for advanced malignancy. It may result from direct extension of a thoracic infection but is more commonly seen as a consequence of a ruptured appendix or bowel perforation by swallowed foreign bodies, such as toothpicks or needles. (iv) Pelvic - It is the most common complication of Intra-uterine contraceptive devices.
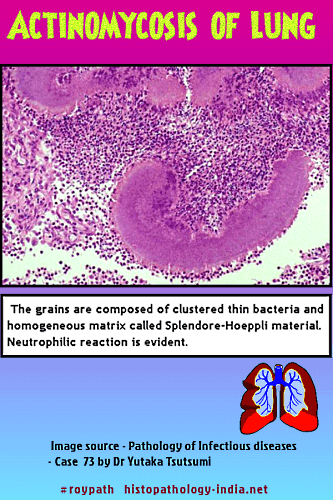
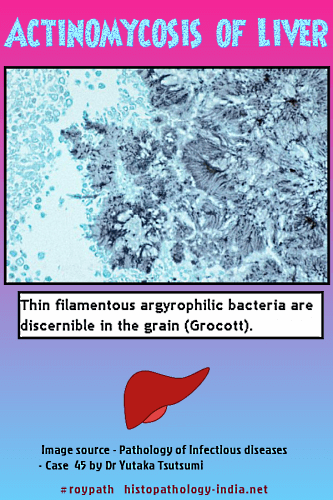
Pathological features: The inflammatory reaction in actinomycosis is suppurative, with formation of abscesses that contain one or more granules (organized aggregates of filaments), 30 to 3000 micrometer in diameter, that are bordered by eosinophilic, club-like, Splendore-Hoeppli material. Bacterial stains reveal that the granules are composed of delicate, branched, gram-positive filaments, about 1 micrometer in diameter, haphazardly arranged in an amorphous matrix of uncertain composition. The filaments may be fragmented and unlike those of the Nocardia species, are not acid-fast. Gomori methenamine-silver staining is also useful for demonstrating the filaments, which are not stained by the hematoxylin and eosin, periodic acid-Schiff and Gridley stains. Specific identification requires culture or immunoflourescence staining because, in tissue sections, the agents of actinomycosis cannot be distinguished from each other. Both gram-positive and gram-negative bacilli and cocci may be found in close association with actinomycete filaments within a granule, but it is generally believed that these bacteria are secondary pathogens.
Histologically, there are chronic granulomas with fibrous stroma and cyst-like spaces containing characteristic granules. Granules are colonies of organisms. Abscess-like granulomas are seen under epidermis which rupture forming sinuses. Treatment: Penicillin is the drug of choice for treating actinomycosis. It is speculated that fewer cases are seen today because of the widespread use of antibacterial antibiotics for treating minor, unrelated infections.
|
|
|
Copyright © 2002-2022 histopathology-india.net