|

Custom Search
|
|
Infectious Disease Online Pathology of Aspergillosis
|
|
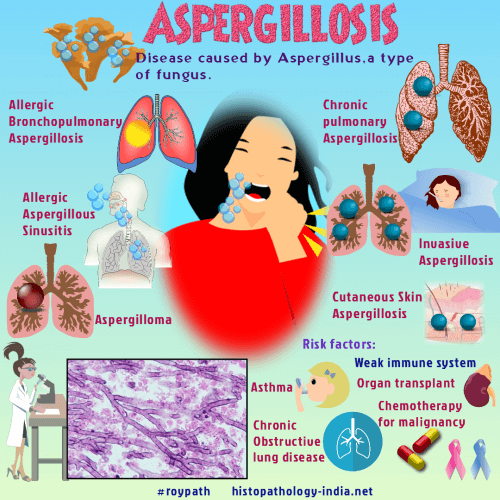
The broad spectrum of disease caused by fungi of the genus Aspergillus includes allergic bronchopulmonary disease, colonization of pulmonary cavities, indolent superficial infection of the skin and mucosal surfaces; chronic, progressive pulmonary infection in mildly compromised hosts and fulminant, invasive pulmonary infection with systemic dissemination in severely immunocompromised patients.
|
|
Aspergillosis is the second most common opportunistic mycosis among patients with malignant disease, accounting for up to 30% of fungal infections and found at autopsy in these patients. A. fumigatus is the species most frequently isolated from patients with invasive or disseminated infection, but A. flavus , A. niger, and other Aspergillus species can also cause disease.
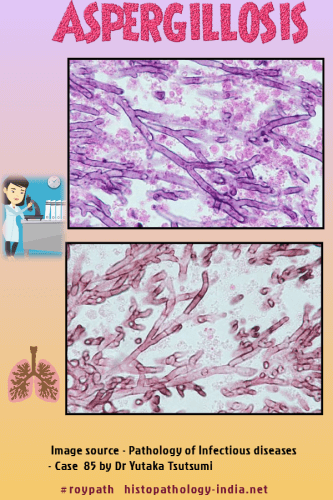
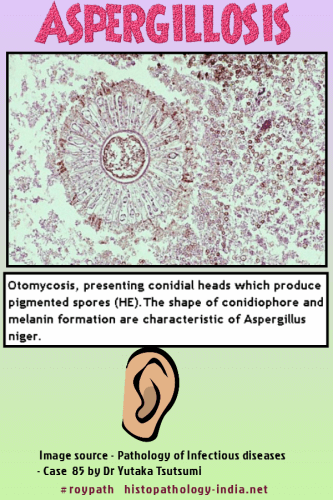
Since the conidia of the aspergilli are ubiquitous in the environment, isolation of an Aspergillus species in microbiologic culture must be interpreted cautiously. Proof of its ecologic role in infection is best confirmed by demonstration of characteristic hyphae in tissue sections. Typical hyphae of the Aspergillus species have a characteristic appearance in the tissue sections. The hyphae are uniform, narrow (3 to 6 micrometer in width), tubular and regularly septate. Branching is regular, progressive, and dichotomous. Hyphal branches tend to arise at acute angles from parent hyphae. Viable hyphae may be deeply basophilic, whereas degenerated or necrotic hyphae are often hyaline or eosinophilic. Hyphal morphology is demonstrated better with the special stains for fungi than with hematoxylin and eosin. Under certain circumstances, the hyphae of the aspergilli may have an unusual or bizarre appearance in tissue sections. Degenerated hyphae encountered in pulmonary fungus balls and in indolent, granulomatous lesions assume bizarre shapes with globose varicosities and inconspicuous septa. Such hyphae may be mistaken for those of the zygomycetes. Conidial (fruiting) heads may be produced in lesions exposed to air, of example, in pulmonary fungus balls and in superficial infections involving the skin and bronchial mucosa. Calcium oxalate crystals may accumulate within the mycelium of fungus balls in the lungs or paranasal sinuses. Hyphal fragments in chronic granulomatous lesions are often coated with eosinophilic Splendore-Hoeppli material. The clinical course and pathologic manifestations of aspergillosis are determined, for the most part, by the integrity of the host defense mechanisms. In the hypersensitized host, the aspergilli can stimulate a variety of allergic pulmonary reactions, which includes the syndrome of allergic bronchopulmonary aspergillosis, chronic eosinophilic pneumonia, mucoid impaction of proximal bronchi, bronchocentric granulomatosis with asthma, and microgranulomatous hypersensitivity pneumonitis. There is considerable clinical and pathologic overlap among these allergic reactions, which seldom occur in pure form. Pathologic findings include mucus hypersecretion, eosinophil infiltration with Charcot-Leyden crystals, bronchiolitis, and destructive granulomatous lesions of the airways. Hyphae, which are difficult to find in these lesions, are fragmented and degenerated, and they do not invade adjacent pulmonary parenchyma or blood vessels. The colonizing form of aspergillosis is typified by the pulmonary aspergilloma, or fungus ball. This is a compact mass of hyphae that forms within a preexisting, usually tuberculous, pulmonary cavity. The clinical diagnosis of aspergilloma is suggested by radiographic demonstration of an intracavitary mass, hemoptysis, and a positive serum precipitin reaction to aspergillus antigens. The mycelial balls measures up to 5 cm in diameter and is composed of tangled, often bizarre hyphae, which may produce conidial heads. Erosion of the cavity wall by the mobile fungus ball results in recurrent or life-threatening hemoptysis, which may necessitate surgical resection of the cavity or involved pulmonary lobe. Because the aspergilli in these lesions are noninvasive colonizers that are confined within the cavity by host defense, antifungal chemotherapy is not required. Fungus balls are occasionally, produced by other fungi, notably Coccidioides immitis and Pseudallescheria boydii. A recently described form of pulmonary aspergillosis, termed chronic necrotizing pulmonary aspergillosis or semi-invasive pulmonary aspergillosis, shares some features of both the colonizing and invasive forms of aspergillosis. It is a locally progressive and destructive infection that occurs in mildly compromised patients who have underlying noncavitary structural lung disease. Chest radiograph disclose parenchymal infiltrates and thick-walled cavities, about 40% of which contain intracavitary fungus balls. Major findings include large cavities that contain fungus balls or amorphous mycelial aggregates, and limited invasion and destruction of adjacent noncavitary lung tissue. Invasive pulmonary aspergillosis is a fulminant opportunistic infection that occurs almost exclusively in patients whose defense mechanisms are severely compromised by hematologic malignancy, corticosteroids, cytotoxic chemotherapy, and granulocytopenia. Clinical findings are nonspecific, and sputum cultures are positive in only about one third of cases. Hyphae proliferate within the bronchial tree, invade through the walls of distal airways, and extend into adjacent arteries and veins. Vascular invasion and thrombotic occlusion result in characteristic nodular infarcts, several millimeters to 3 cm or more in diameter, that may replace much of a lobe. Each of these nodules is composed of a central zone of fibrinous exudates, and a peripheral zone of parenchymal hemorrhage. Hyphae radiate throughout these nodules from a central, occluded blood vessel. Hyphal invasion and occlusion of larger, proximal arteries and veins, results in large wedge-shaped hemorrhagic infarcts. Suppurative bronchopnneumonia may occur in nongranulocytopenic patients. Disseminated infection develops in about 25% of patients with invasive pulmonary aspergillosis. The gastrointestinal tract, central nervous system, heart, kidneys, and liver are frequently involved, but lesions may be found in any organ. The systemic lesions are infarctive, less often suppurative or granulomatous. Endocarditis of native or prosthetic cardiac valves results in bulky, friable vegetations and is usually accompanied by myocardial lesions. The aspergilli cause a variety of indolent, superficial infections in mildly compromised hosts. Localized granulomatous infections can occur in the lungs, subcutaneous tissue, paranasal sinuses and orbit of diabetics or patients treated with corticosteroids. Cutaneous lesions may result disseminated infection or can occur primarily in burned patients. The aspergilli also cause superficial infections of the external ear canal and nails. Other pathogenic fungi that form branched, septate hyphae can be mistaken for the aspergilli in tissue sections. These fungi include Pseudallescheria boydii, the Fusarium species and, on occasion, the Candida and the zygomycetes. Recognition of subtle differences in the morphology of these fungi may enable one to differentiate them from the aspergilli. However, unless typical conidial heads are observed, a histopathologic diagnosis of aspergillosis must be considered presumptive unless confirmed by direct immunoflourescence or microbiologic isolation of Aspergillus from the lesion.
|
|
|
Copyright © 2022 histopathology-india.net

