|

Custom Search
|
|
Infectious Disease Online Pathology of Buruli Ulcer (Mycobacterium ulcerans) "A Neglected Emerging Tropical Disease considered third most common Mycobacterial disease."
|
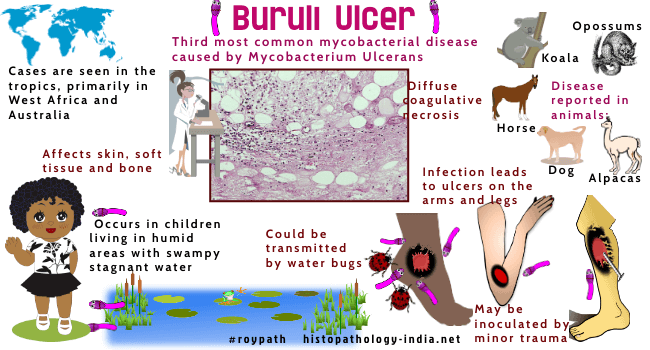
| It is the
third most common mycobacterial disease in immunocompetent people and
affects mainly children living in humid areas of the tropical rain
forest.
First described as a rare disease in Australia, these ulcers are now recognized as common in Uganda and Zaire and have been identified in other countries of West Africa, as well as in South East Asia and central and South America. The name is derived from Buruli Country in Uganda, where a cluster of patients was identified in late 1950s. The reservoir and route of infection are unknown, but organisms are probably inoculated by minor penetrating trauma. The major endemic areas are sparsely populated river valleys and swampy low-lands. Buruli ulcers are caused by Mycobacterium ulcerans, an acid-fast bacillus that grows slowly on routine mycobacteriological media at several degrees below body temperature. Ecology and Transmission of Buruli Ulcer Disease: A Systematic Review Most Buruli ulcers are on the limbs, frequently over joints. The bacilli proliferate in the skin and subcutaneous tissues and elaborate a cytotoxin that diffuses symmetrically and causes a contiguous necrosis of all structures in its path - (the epidermis, dermis, panniculus, deep fascia, nerves, vessels, and (rarely) underlying muscle and bone). These lesion begins as a firm, painless, subcutaneous nodule that becomes papular and ulcerates. The perimeter of the ulcer is typically scalloped and often deeply undermined. At first the ulcers spread steadily, under the skin over large areas. After many months the perimeter stabilizes and healing begins, a process that requires many months. The eventual scar is broad and depressed and resembles a healed third degree burn.
Preulcerative infections may be cured by local wide excision. When excision is impractical, the most effective therapy is repeated debridement and grafting, combined with continuous heating of the area to 40 degree centigrade, using a circulating water jacket. Rifampin is the chemotherapeutic agent of choice.
|
|
|
Copyright © 2022 histopathology-india.net

