|

Custom Search
|
|
Infectious Disease Online
Pathology of Cholera
|
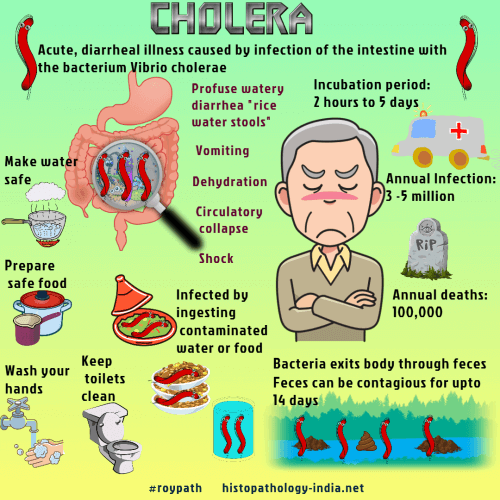
Cholera is caused by the enterotoxin elaborated by Vibrio cholerae, a gram-negative bacillus.The organism proliferates in the lumen of the small intestine and causes profuse watery diarrhea, rapid dehydration, and (if fluids are not restored) shock and death within 24 hours of the onset of symptoms.Enterotoxins of other vibrios (for instance Vibrio parahemolyticus) also cause diarrhea and mimic cholera, but symptoms are milder.In the 19th century cholera was common in most parts of the world, but it periodically “disappears”. There have been major pandemic - (1961-74) : Extended throughout Asia, the Middle East, southern Russia, the Mediterranean basin, and parts of Africa. Vibrio cholerae is a curved gram-negative bacillus with a polar flagellum that moves in a helical path, with a characteristic wobble. Vibrio cholerae is destroyed by gastric acid. Successful colonization in the small intestine depends on (a) a reduction or dilution of gastric acid, (b) bacterial motility, pili, and production of enzymes (colicins, mucinase, neuraminidase), and (c) availability of binding sites for the organisms and the enterotoxin. Pathogenic strain adhere to cells of the intestinal mucosa. Drinking water contaminated with Vibrio cholerae and food prepared with contaminated water are infectious. Those with a normal gastric acidity are much less susceptible than those with low levels of stomach acid as result of a gastrectomy or other cause. Vibrios traverse the stomach, enter the small intestine and propagate. They remain in the lumen and do not invade the intestinal mucosa. They do, however elaborate an enterotoxin, which contains A and B subunits. The B subunit binds the toxin to GM1 ganglioside in the cell membrane at the brush border of the small intestine. The A subunit enters the cell and activates adenyl cyclase, thereby initiating a chain of reactions in the membrane. Symptoms begin when the massive secretion of water and sodium in the small intestine, a consequence of the activation of cyclic AMP, exceeds the resorptive capacity of the colon. The small intestine, however, is not damaged morphologically either by the vibrios or by the enterotoxin. The loss of sodium and water causes severe diarrhea, called “ricewater stool”. Fluid loss may exceed 1 liter per hour. Acute dehydration , hypovolemic shock, and metabolic acidosis follow quickly. The patient exhibits dry skin, sunken eyes, lethargy, cyanosis, a weak pulse, faint heart sounds, hemoconcentration, and elevation of serum proteins. The hematocrit may rise to 55-65 and the plasma specific gravity to 1.035-1.050. Patients are usually afebrile, body temperature may be subnormal. Treatment is prompt rehydration, and under such circumstances most patients survive. After the onset of diarrhea, urine production ceases, but renal function improves when fluid and electrolytes are replaced. Inadequate replacement, however, leads to prolonged renal failure, with acute damage of tubules and the vacuolar lesions of hypokalemia. For many years, the intestinal changes in cholera could be studied only at autopsy. Degenerative changes in the intestinal epithelium, although observed repeatedly in victims of cholera, could not be distinguished from the autolysis that begins in the intestine at the moment of death. Specimens of the small intestine taken promptly after death have now shown that cholera patients have an intact intestinal epithelium and, except for minor, nonspecific changes, a morphologically normal mucosa.
|
|
|

