|
Coccidioidomycosis is caused by
the dimorphic fungus Coccidioides immitis.
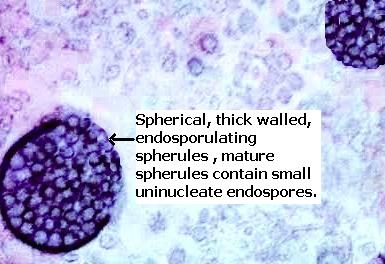
The organism is thick-walled, mature, spherules containing endospores.
Spherules rupture liberating endospores into surrounding tissue.
It causes
chronic, necrotizing lesions that clinically & pathologically resembles
tuberculosis.
High risk groups are
African-Americans and Asians, pregnant women during the third trimester, and
immunocompromised persons.
Construction or agricultural
workers, and archeologists who are exposed to dust are also at risk.
Epidemiology:
Endemic in
the south-western United States, parts of Mexico and South America.
Reservoir :
Soil in semiarid areas.
  (Enlarged view of the infographic)
(Enlarged view of the infographic)
Mode of infection:
Inhalation of airborne arthroconidia (barrel shaped infectious units) from
contaminated soil.
The contaminated soil may be disturbed
following excavation or after a natural disaster like dust storm or
earthquake.
Arthroconidia mature to form endospore containing
spherules.
Presentation:
A- 60% of air born infections are
asymptomatic.
B- 40% cases are symptomatic.
Lung: Primary pulmonary coccidioidmycosis are acute disease with influenza-like symptoms associated
with suppurative or granulomatous pneumonitis with abundant organisms.
Initially, there is a solitary area of consolidation, sometimes diffuse
pneumonic consolidation or multiple foci of consolidation is seen.
Cavitation is the most common
complication, which may communicate with bronchial tree.
Hilar lymph nodes may or may not be involved.
Disseminated lesions (0.5-1% of patients) by hematogemous route are seen in meninges,
skin, soft tissue, bones, adrenals,
spleen, liver.
Meninges:
Central nervous system is affected in
50% patients with disseminated lesion.
Coccidial meningitis is a chronic lesion with
insidious onset.
Granulomatous and suppurative lesions are noted affecting basilar process
and sometimes brain parenchyma and spinal cord.
Hydrochephalus is a
complication.
Skin:
Primary infection is very rare following
inoculation of organisms at sites of trauma.
In disseminated disease the skin lesions
takes the form of verrucous
plaques (nasolabial fold), granulomatous papules and nodules usually on the
head.
Subcutaneous abscesses or pustular lesions
and sinus tracts are also
noted.
Joints:
Synovitis
and effusion. Usually knee, ankle and wrist joints are involved.
Bones:
Chronic
osteomyelitis. Long bones as well as bones of hands, feet, pelvis and skull
may be involved.
Other organs involved include:
Thyroid,
gastrointestinal tract, genito-urinary tract, pericardium and peritoneum
Microscopic features:
In tissue the
inflammatory reaction is both purulent and granulomatous.
Endospores
incite a polymorphonuclear response.
As the endospores mature into
spherules, the acute reaction is replaced by lymphocytes, plasma cells,
epithelioid cells and giant cells.
Lungs: Caseative pulmonary granuloma
(resemble Tuberculosis),
Epithelioid cells and
giants cells may be noted,
Organisms are present within the granuloma,
Mature spherule with endospores,
Hyphae may be present
in the pulmonary cavities,
Often associated with
microabscess formation,
Most
of the lesions are healed by fibrosis & calcification.
Skin: Non caseating granuloma in the upper and mid-
dermis,
Thick walled spherules within the granuloma,
Early
lesions and subcutaneous abscesses demonstrate abundant neutrophil
polymorphs,
Some lymphocytes, histiocytes and eosinophils are also
present.
Laboratory diagnosis:
1. Skin test ;
2. Serodiagnosis ;
3. Immunoflourescence- confirmatory.
|


