|
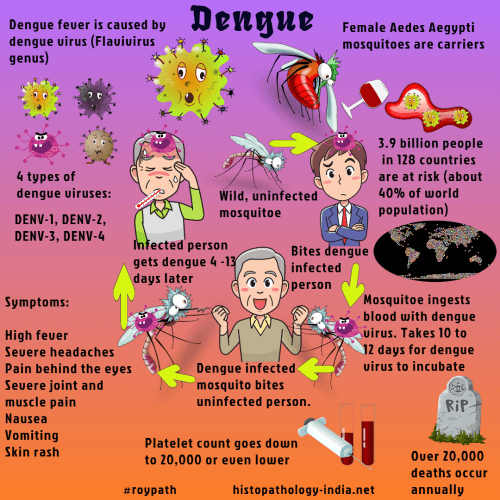
Dengue the most prevalent arthropod-borne viral (Arborvirus)
disease of humans caused by
four serotypes of dengue virus (DENV 1-4) of the genus Flavivirus.
It is transmitted
to man by mosquito Aedes aegypti.
It is common in
tropical and subtropical countries, especially in coastal areas.
In terms
of numbers of individuals infected, it is by far the most devastating of all
the recognised arthropod-transmitted virus diseases. It is estimated that
more than 3 billion humans live in dengue endemic regions of the world, and
currently, more than 50 million infections occur annually with at least
500,000 individuals requiring hospitalisation.
Source: Man is infective to mosquito and mosquito transmits the disease to man.
Clinical presentation:
Clinically, symptoms start 6 days after infection
as malaise and headache, followed by sudden onset of fever, intense backache
and generalized pains, mainly in the orbital and periarticular areas.
After
an afebrile interval of 24 to 48 hours, there is recurrence of fever for a
day or two (‘saddleback fever’).
There may be skin rash and lymphadenopathy.
In persons, previously exposed to
Dengue virus, antiviral antibodies may enhance the uptake of virus into host
cells and cause disseminated intravascular coagulation, shock and death
(hemorrhagic
dengue).
Pathological features:
Biopsy studies of the rash seen in nonfatal dengue fever
show a lymphocytic vasculitis in the dermis.
In cases of
fatal dengue hemorrhagic fever the
gross findings are petechial hemorrhages in the skin and hemorrhagic
effusions in the pleural, pericardial and abdominal cavities.
Hemorrhage and
congestion are seen in many organs.
Histopathological examination show
hemorrhage, perivascular edema and focal necrosis but no vasculitic or
endothelial lesions.
It is believed that most of the morphologic
abnormalities seen result from disseminated intravascular coagulation and
shock.
Differential diagnosis
:
Includes malaria , typhoid fever, leptospirosis, West Nile
virus infection, measles , rubella, acute human immunodeficiency
virus conversion disease, Epstein–Barr virus infection, viral
hemorrhagic fevers, rickettsial diseases, early severe acute
respiratory syndrome (SARS), and any other disease that can
manifest in the acute phase as an undifferentiated febrile
syndrome.
Diagnosis:
A
confirmed diagnosis is established by culture of the virus,
polymerase-chain-reaction (PCR) tests, or serologic assays.
The diagnosis of dengue
hemorrhagic fever is made on the basis of the following triad of
symptoms and signs:
- Hemorrhagic manifestations;
-
A platelet count of less than 100,000
per cubic millimeter; and
- Objective evidence of plasma leakage,
shown either by fluctuation of packed-cell volume (greater than
20 percent during the course of the illness) or by clinical signs
of plasma leakage, such as pleural effusion, ascites, or
hypoproteinemia.
Hemorrhagic manifestations without capillary
leakage do not constitute
dengue
hemorrhagic fever.
|