|

Custom Search
|
|
Dermpath-India Pathology of Fibrous Hamartoma of Infancy
|
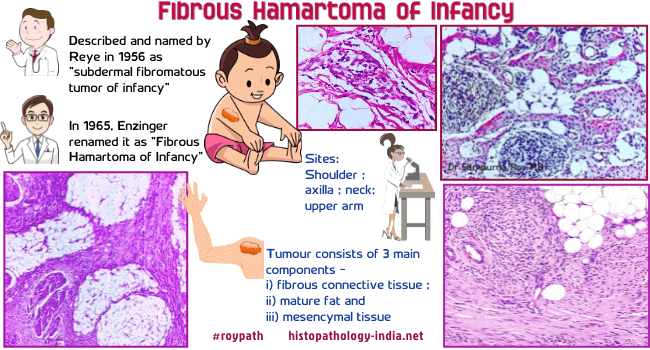
This tumour was previously known as 'subdermal fibromatous tumour of infancy'. It was called 'fibrous hamartoma of infancy' by Enzinger in 1965. Age: Usually occurs in the first two years of life. The tumour may be present since birth or in some cases present in older children. Site: Shoulder, axilla, neck and upper arm. Cases have been reported in the perianal area, scrotum and the inguinal region. Clinical presentation: Presents as a painless solitary, at times rapidly growing nodule. Multiple lesions have been reported. There is a male predominance of 3:1. The clinical course is benign, despite its infiltrative appearance and tendency to recur. The tumour shows no evidence of malignant transformation . Gross appearance: Firm circumscribed poorly defined fibro-fatty tissue usually present in the deep dermis and subcutis. Cut surface has a glistening gray-white appearance interspersed with fatty tissue. The involved area measures 2-8 cm in maximum diameter. Microscopic features : The tumour has a poorly defined margin. There are some reports of older lesions showing some encapsulation. The lesion is centred on the subcutis. The three main components are: 1. Interlacing trabeculae of dense fibrocollagenous tissue. Finger like projections of fibrous tissue extend into the fatty tissue. 2. Small round to ovoid nests of undifferentiated spindle or stellate cells set in a myxoid stroma containing delicate vessels. The mucoid matrix is Alcian blue positive. Sparse lymphocytes may be present in the stroma. 3. Interspersed mature adipocytes. The fat tissue varies from case to case and is much greater than normally present in the subcutis. Extension into underlying tissue, like muscle or fascia, is a known feature, but visceral involvement has not been reported. An unusual pseudoangiomatous histologic pattern has been reported. Immunohistochemistry: Routine hematoxylin-eosin stained sections are generally sufficient for a diagnosis, but immunochemistry may be useful. Immunohistochemical analysis show reactivity for smooth muscle actin and CD34 in the mature fibrous tissue, S100 protein in the mature adipose tissue, and variable CD34 reactivity in immature mesenchymal and pseudoangiomatous foci. In some cases Ki-67 proliferative activity is noted in the immature mesenchymal and pseudoangiomatous foci and Bcl-2 reactivity restricted to mesenchymal and pseudoangiomatous foci. Differential diagnosis: 1. Lipofibromatosis: Rare pediatric soft tissue tumour recently classified as lipofibromatosis by Fetsch et al. Histologically, these tumors have abundant adipose tissue traversed by bundles of fibroblast-like cells. Nests of immature cells in a myxoid matrix are typically lacking in these tumors as compared to fibrous hamartoma of infancy. A Clinicopathologic Study of 45 Pediatric Soft Tissue Tumors With an Admixture of Adipose Tissue and Fibroblastic Elements, and a Proposal for Classification as Lipofibromatosis. 2. Infantile digital fibromatosis: Occurs almost exclusively in the fingers and toes. These tumor cells are characterized by intracytoplasmic perinuclear eosinophilic inclusions. 3. Calcifying aponeurotic fibroma: This lesion shows characteristic histologic pattern called zonation - Calcific areas are surrounded by hyalinized collagenous foci, which in turn are palisaded by plump fibroblasts. This tumour may not exhibit foci of calcification in its earliest phase and often infiltrates fat in infants and young children. The absence of immature mesenchyme and trabecular arrangement of fibroblasts distinguishes this from fibrous hamartoma of infancy. Calcifying aponeurotic fibroma: a clinicopathologic study of 22 cases arising in uncommon sites. 4. Myofibromas: This lesion is commonly found in the head and neck region and trunk. Histologically, the lesion appears biphasic with alternating light- and dark-staining areas. The dark-staining areas are composed of bundles of myofibroblasts exhibiting a hemangiopericytoma-like pattern. 5. Dermatofibroma: 6. Neural fibrolipoma: 7. Nodular fasciitis: This lesion is rare in children, circumscribed with abundant proliferation of plump fibroblasts , frequent mitoses and extravasated erythrocytes. 8. Dermatofibrosarcoma protuberans (plaque form): Early to middle adult life. Characterized by uniform slender fibroblasts in a storiform pattern, areas of higher mitotic activity with nuclear atypia. Immunohistochemistry - CD34: positive Benign, soft tissue tumour in infants -Fibrous Hamartoma of Infancy [Pathology Infographic]
|
|
|


