|

Custom Search
|
|
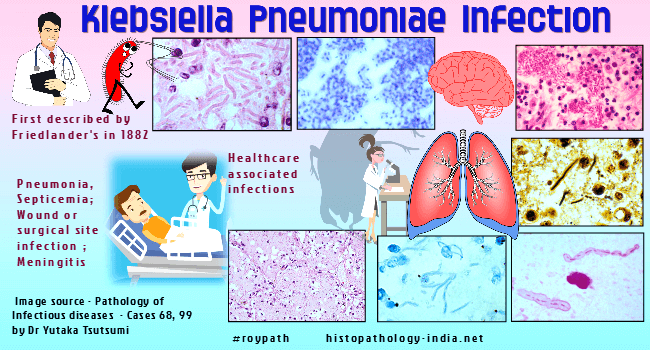
Infectious Disease Online Pathology of Klebsiella Pneumoniae Infection
|
|
Klebsiella pneumoniae, (previously known as Friedlanderís bacillus), is a short, encapsulated, gram-negative bacillus that can cause different types of healthcare-associated infections, including pneumonia, bloodstream infections, wound or surgical site infections, and meningitis. This organism also causes 10% of all infections acquired in hospital, including pneumonia and infections of the urinary tract, biliary tract, and surgical wounds. Carriers are a special hazard among hospital personnel, especially when resistant strains of Klebsiella pneumoniae colonize their mouths, throats, and intestines. Predisposing factors are indwelling catheters and endotracheal tubes, old age, alcoholism, immunosuppression, diabetes, congestive heart failure, obstructive pulmonary disease, and other debilitating conditions. Furthermore, secondary Klebsiella pneumonias may complicate influenza or other viral infections of the respiratory tract. The combined mortality rate of primary and secondary Klebsiella pneumonias is about 50%, because the necrotizing pneumonia is itself dangerous and because those stricken tend to be chronically ill or otherwise debilitated. Clinically, the pneumonia has a sudden onset, characterized by fever, pleuritic pain, cough, and thick mucoid sputum when infection is severe these symptoms progress to shortness of breath, cyanosis,and death in 2 to 3 days. The thick blood tinged sputum resembles "red currant jelly". Pneumonia develops when the bacilli invade and multiply within the alveolar spaces. The pulmonary parenchyma becomes consolidated, and the mucoid exudates that fills the alveoli is dominated by macrophages, fibrin, and edema fluid. Neutrophils are inhibited by a neutral polysaccharide in the capsule of Klebsiella pneumoniae, and are not a significant part of the early exudates. Numerous encapsulated gram-negative bacilli appear free in the exudates and in alveolar macrophages. As the exudates accumulates the alveolar wall become compressed and then necrotic. Numerous small abscesses may coalesce and lead to cavitation. The pneumonia, or other infections by Klebsiella pneumoniae, may be complicated by a fulminating, often fatal, septicemia, even without disseminated lesions in other tissues. Diagnosis is made by culture. Both an aminoglycoside and a cephalosporin are recommended for treatment.
|
|
|

