|

Custom Search
|
|
Infectious Disease Online Pathology of Legionellosis (Legionnaires' disease) |
|
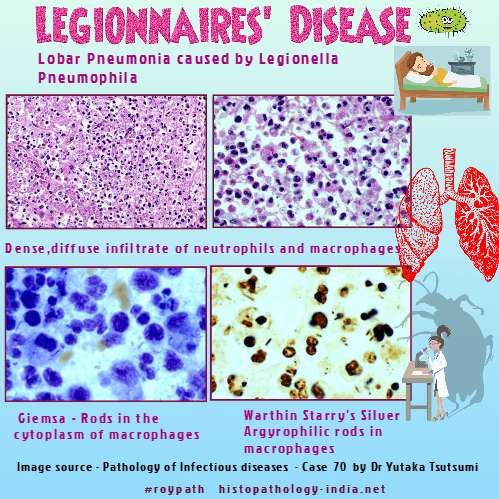
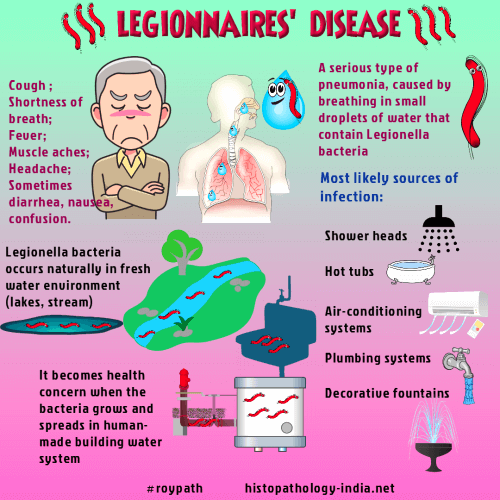
Legionnaires' disease (Legionellosis) is an acute bacterial infection, caused by Legionella pneumophila (a minute, gram-negative bacillus), which involves primarily the lower respiratory tract, although it is often associated with multi-systemic extrapulmonary manifestations. Afflicted patients may sometimes have gastrointestinal symptoms, liver function abnormalities, renal failure, central nervous system complications and cutaneous manifestations which may include erythematous, maculopapular or petechial skin lesions. About 6 months after an outbreak of a severe respiratory disease of unknown cause at the American Legionís state convention in Philadelphia in 1976, Legionella pneumophila was identified by workers at the Centers for Disease Control. Subsequently, retrospective serologic and immunoflourescent studies revealed antibodies in sera from previously unexplained epidemics. Of historical note is the first epidemic so recognized, in a meat packing plant in Minnesota in 1957. Legionnairesí disease occurs sporadically, as epidemics, and as nosocomial infections, especially in patients with compromised immunity. Those who abuse alcohol and smoke heavily are also at increased risk. The organism has been recovered from soils, ponds, water systems, and air conditioning systems. Legionellosis has been recognized throughout the world, without a geographic pattern. The disease presents as a rapidly progressive, severe, necrotizing pneumonia, accompanied by fever, nonproductive cough, and myalgias. The onset is abrupt, after an incubation period of 2 to 10 days. Within 2 days, most patients develop a persistent high fever and respiratory rales. Radiograms of the chest reveal unilateral, diffuse, patchy broncho- pneumonia, progressing to widespread nodular consolidation, usually without cavitation.
Toxic symptoms and hypoxia may be prominent, and death may follow in a few days. In those who survive, convalescence is prolonged. The antibiotic of choice is erythromycin. The main changes in the lung include consolidation, necrosis, and acute congestion. Microscopically, the alveoli are packed with an exudate composed of histiocytes and fibrin. The alveolar walls become necrotic and are destroyed. Neutrophils accumulate as necrosis becomes more pronounced and eventually confluent. Many histiocytes show eccentric nuclei, pushed aside by cytoplasmic vacuoles containing Legionella pneumophila. Dissemination of Legionella pneumophila to the kidneys, spleen, bone marrow, and lymph nodes has been reported. Isolation and identification of the bacilli is necessary for an unequivocal diagnosis, but isolation may be hazardous. The direct fluorescence antibody test for Legionella pneumophila can be performed on formalin-fixed, paraffin-embedded tissue and is thus valuable for conforming the diagnosis.
|
|
|