|

Custom Search
|
|
Infectious Disease Online Pathology of Listeriosis
|
|
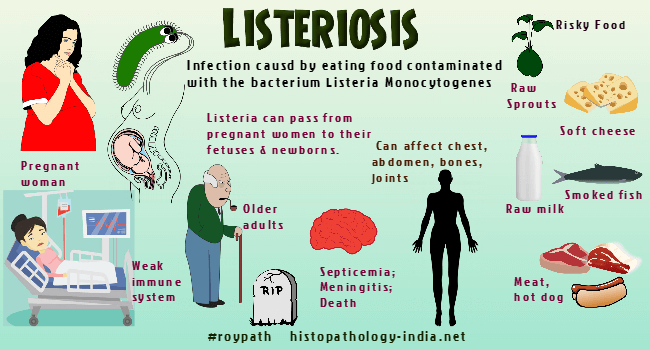
Listeriosis is a systemic infection caused by foodborne pathogen Listeria monocytogenes, a small, motile, nonsporulating, hemolytic, gram-positive coccobacillus. On cultures the organism is easily confused with streptococci or corynebacteria. Predisposing factors: Listeriosis is the leading food-borne fatal infection affecting most often the immunocompromised, the elderly, pregnant women and neonates. Newborns can acquire the infection in utero or during passage through the birth canal, and are acutely ill with multiple organ involvement and symptoms of either pneumonia or meningitis. Listeriosis is a severe disease with high hospitalization and case fatality rates. It is usually sporadic but may also be epidemic. It is usually asymptomatic or very mild in other (immunologically normal) individuals. Listeria monocytogenes can survive and grow over a wide range of environmental conditions such as refrigeration temperatures, low pH and high salt concentration. This allows the pathogen to overcome food preservation and safety barriers, and pose a potential risk to human health. Outbreaks of listeriosis have been caused by unpasteurized milk, contaminated cheeses and other dairy products. Raw vegetables can also transmit the disease. Distribution: Listeria monocytogenes has been isolated worldwide from surface water, soil, vegetation, the faeces of healthy people, from many species of domestic and wild mammals, and from several species of birds. Inspite of this wide distribution, the spread of infection from animals to humans is rare. Most human infections are in urban rather than rural environments and occur during July and August, while the peak months of infections in animals are January through May. Mode of infection: The organism initially colonizes the intestinal epithelium, then enters the macrophages and spreads hematogenously. It enters cells by induced phagocytosis, then escapes the phagosome by means of the virulence factor, listeriolysin, and grows in the cytoplasm. Using the cell's actin transport system, it spreads directly from cell to cell. Most infections fall into one or two groups: 1. Listeriosis of pregnancy, includes prenatal and postnatal infections. 2. Listeriosis of the adult population, is characterized by meningoencephalitis and septicemia. Chronic alcoholics, patients with carcinoma, leukemia, or lymphomas and those receiving immunosuppressive therapy are all susceptible. Maternal infection early in pregnancy leads to abortion or prematurity. Infected live-born, premature infants show signs of infection within a few hours of birth. These signs include respiratory distress, pneumonia, hepatosplenomegaly, papular cutaneous and mucosal nodules, leukopenia, and thrombocytopenia. In neonatal listeriosis acquired during delivery, the onset is 3 days to 2 weeks after delivery. Infections before birth involve many organs and tissues. The amniotic fluid, the placenta, and cord are all heavily infected. The cutaneous lesions are raised and necrotic with red margins. Abscesses are found in the liver, spleen, lymph nodes, adrenals, lungs, pleura, esophagus, posterior pharynx and tonsils. Microscopically, the visceral lesions are foci of necrosis and suppuration that contain many bacteria. Older lesions contain histiocytes and occasionally epithelioid cells and lymphocytes, but not giant cells. Still older lesions have a fibrous wall. Neurologic sequelae are common, and the mortality is high even when therapy is prompt. Meningitis is the most common form of listeriosis in adults, and resembles other bacterial meningitides. Microscopically, the leptomeninges are infiltrated with lymphocytes, plasma cells, macrophages, and neutrophils. The inflammation extends into the brain along the Virchow-Robin spaces. Septicemic listeriosis in adults is most common in immunodeficient patients, and causes severe illness with high fever and prostration. Shock and disseminated intravascular coagulation may lead to an erroneous diagnosis of gram-negative sepsis. Listerial endocarditis resembles endocarditis caused by other bacteria. Septicemia may seed the brain with military abscesses and cause a suppurative leptomeningitis. Diagnosis : The diagnosis is made by isolating L. monocytogenes in culture or demonstrating the typical gram-positive bacilli in tissue sections. Treatment : Prolonged treatment with antimicrobials is usually required, because patients tend to relapse if treatment is less than 3 weeks. Penicillin or ampicillin is the treatment of choice.
|
|
|

