|

Custom Search
|
|
Infectious Disease Online Pathology of Mucormycosis (Zygomycosis)
|
|
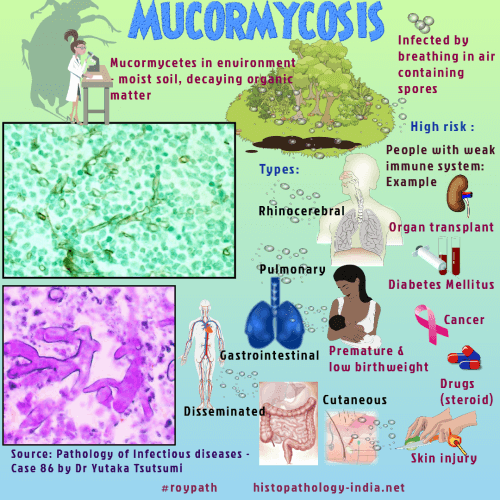
Mucormycosis (previously called zygomycosis) is a rare, potentially life-threatening, angioinvasive fungal infection. The class Zygomycetes is divided into two orders, Mucorales and Entomophthorales. Types of fungi that commonly cause mucormycosis - Caused by infection with fungi in the order Mucorales (Rhizopus, Mucor, Rhizomucor, Lichtheimia , Apophysomyces, Cunninghamella and Syncephalastrum). Types of mucormycosis - Mucormycosis presents with rhinocerebral, pulmonary, disseminated, cutaneous, or gastrointestinal involvement. Risk factors -Immunocompromising states such as haematological malignancy, bone marrow or peripheral blood stem cell transplantation, neutropenia, solid organ transplantation, diabetes mellitus with or without ketoacidosis, corticosteroids, and deferoxamine therapy for iron overload predispose patients to infection. Mucormycosis in immunocompetent hosts is rare, and is often related to trauma. Mortality rates can approach 100% depending on the patient's underlying disease and form of mucormycosis. Mode of infection: These saprophytic fungi are widely distributed in nature and infection is acquired by exposure to their sporangiospores. Although relatively uncommon, mucormycosis is the third most frequent opportunistic mycosis in patients with neoplastic diseases. Appearance of the hyphae: The hyphae of the mucoraceous zygomycetes have a characteristic appearance in tissue sections. Typical hyphae are broad (6 to 25 micrometer wide), thin-walled and pleomorphic, with irregular, non-parallel contours. Branches arise haphazardly, often at right angles to the parent hyphae. Septa can be found in some of the hyphae, though most of the hyphae appear nonseptate (cenocytic). Because the hyphae have little structural stability, they are often folded, twisted, wrinkled, or collapsed. The thin hyphal walls stain as well with hematoxylin as with the special stains for fungi. Thick-walled, ovoid chlamydoconidia are rarely formed in tissues , but sporangia are almost never produced. Clinical presentation: Several clinical forms of mucormycosis are recognized. Rhinocerebral mucormycosis begins as a fulminant infection of the nasal cavity, paranasal sinuses, and soft tissues of the orbit. The infection, often unilateral, may extend directly from these sites to involve the meninges and brain, and it may be complicated by thrombosis of the cavernous sinus and internal carotid artery. Patients with diabetic acidosis or leukemia are predisposed to rhinocerebral infection, which is most often caused by Rhizopus oryzae. Once established, this infection is difficult to treat and is rapidly fatal. Invasive pulmonary mucormycosis and disseminated mucormycosis occur preferentially in patients with acute leukemia or lymphoma. A more limited endobronchial form, which occurs in diabetics, causes bronchial obstruction and may eventually lead to serious hemorrhage after hyphal invasion into adjacent blood vessels. Gastrointestinal mucormycosis usually begins as a secondary infection of preexisting ulcers in malnourished persons, but it may also be a manifestation of disseminated infection. The stomach is involved most frequently, followed by the colon and small intestine. Cutaneous mucormycosis can be a manifestation of disseminated mucormycosis or can occur as a primary infection of burned patients or patients whose surgical wounds are dressed with contaminated elastic bandages. Many of the bandage-associated nosocomial infections have been caused by Rhizopus rhizopodiformis. Disseminated mucormycosis can involve almost any organ, most frequently the lungs, central nervous sysytem, spleen, kidneys, heart, and gastrointestinal tract. Septic thrombosis of the coronary arteries produces mycotic myocardial infarction. Pathological features: Pulmonary mucormycosis is a progressive infection characterized by pulmonary vascular invasion, parenchymal infarction, and hematogenous dissemination. In gastrointestinal mucormycosis mucosal lesions are blackened, necrotic ulcers, and local vascular invasion may lead to ischemia of adjacent segments of the stomach or intestine. Cutaneous lesions are necrotic nodules that ulcerate and become covered with blackened exudates. Invasive opportunistic infections caused by the mucoraceous zygomycetes are characterized by tissue infarction and, in the non-granulocytopenic host, acute suppurative inflammation. Infarcts are caused by thrombosis complicating hyphal invasion of arteries and veins. Angioinvasion may also lead to hematogenous dissemination. Microscopically, the lesions are characterized by coagulative necrosis and neutrophilic infiltration. Rarely a granulomatous reaction is observed in localized, indolent, or partially treated infections. Treatment: Successful treatment of mucormycosis depends on early recognition of the infection and control of the underlying disease coupled with radical debridement or excision of devitalized tissue and systemic antifungal chemotherapy with amphotericin B. Prognosis: Greater awareness of this opportunistic infection and rapid clinical intervention have resulted in improved prognosis.
|
|
|

