|

Custom Search
|
|
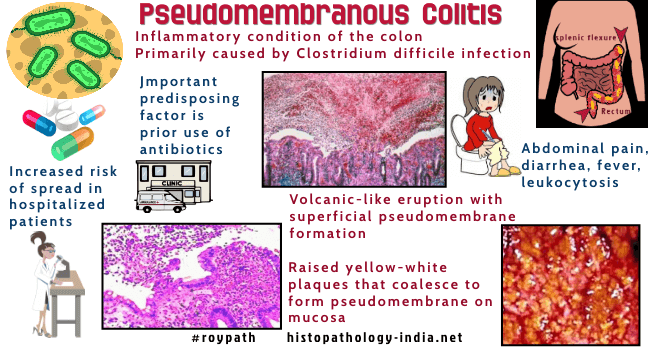
Infectious Disease Online Pathology of Pseudo-membranous Colitis (Antibiotic Associated Colitis or Clostridium Difficile Colitis )
|
|
Pseudomembranous colitis (PMC) is an acute colitis characterized by the formation of an adherent inflammatory membrane (pseudomembrane) overlying sites of mucosal injury. Pseudomembranous colitis is a well recognised cause of diarrhea in patients following a course of broad-spectrum antibiotic therapy. Clostridium difficile infection is the most important infectious cause of PMC. Pseudomembranous colitis may rarely appear after surgery (Example: Following resection for Hirschsprung's disease) or superimposed on a chronic debilitating disease. It has also been suggested to be related to collagenous colitis. It was first described in a woman with severe diarrhea who died shortly after gastric surgery and was found to have "diptheritic colitis" at autopsy. (Bull John Hopkins Hosp. 1893: 4:53). For many years it was believed that Pseudomembranous colitis was caused by staphylococci. In 1977 it was established that Pseudomembranous colitis was caused by toxins produced from Clostridium difficile- a gram positive anaerobic bacillus. Toxin A (enterotoxin) and toxin B (cytotoxin) are produced by C. difficile and are involved in the disease process. Pseudomembranous colitis is frequently nosocomial with an increased risk of spread among hospitalized patients. All groups of antibiotics like cephalosporin, penicillin, clindamycin and ampicillin are commonly associated with pseudomembranous colitis. Elderly patients are more commonly affected in this condition. Clinical manifestations may vary from mild diarrhea to fulminant colitis. Other constitutional symptoms include low grade fever, nausea, vomiting, localised pain and dehydration. Serious complications of fulminant colitis include perforation and development of toxic megacolon. Antibiotic- associated colitis implies a clear history of antibiotic therapy and biopsy evidence of colitis with or without formation of pseudomembrane. Antibotic-associated diarrhea (AAD) is a milder form of disease and is characterized by self limiting diarrhea following use of antibiotics with normal biopsy findings. The diarrhea is usually due to changes in the composition and function of the intestinal flora. Features considered nonspecific but suggestive of Clostridium difficile infection include leukocytosis, hypoalbuminemia and faecal leukocytes and occult blood. Cytotoxin assay using tissue cultured cells is considered the most accurate diagnostic test for detection of C. difficile. The patient promptly respond to treatment but relapses are common. Surgical intervention is indicated in complicated cases of fulminant colitis. Pathological features of Pseudomembranous colitis: Gross features: Macroscopically there are discrete cream to yellow coloured plaques which vary in size between 2 to 20 mm. These plaques are usually loosely attached to the erythematous bowel wall. The pseudomembranes can be easily removed during endoscopy. The intervening mucosa may show hyperemia, edema and superficial erosion. In advanced cases the pseudomembranes are more confluent and linear ulcers develop. Histological features: The earliest feature in Pseudomembranous colitis is small surface erosion of the superficial colonic crypts and overlying accumulation of neutrophils, fibrin, mucus and necrotic epithelial cells (summit lesion). The inflammatory exudate erupts from the superficial degenerating crypts in an explosive or mushroom-like configuration. The lamina propria adjoining the area of necrosis has an infiltrate of neutrophils and eosinophils. The inflammatory debris and neutrophils are present in a linear fashion within the fibrin and mucin. In advanced lesion there is necrosis of superficial crypts with a more dense infiltrate of neutrophils and a plaque like pseudomembrane of neutrophils, fibrin and cellular debris covering the mucosal surface. Most lesions involve superficial mucosa. Rarely deep denuding ulcers may be present. In antibiotic associated colitis with no membrane, histologically the surface epithelium appears crenated and focally heaped up. There is a superficial infiltrate of neutrophil polymorphs in the lamina propria. Nuclear debris is noted together with capillary dilatation and superficial edema. The pathologist must examine further deeper levels to exclude the possibility of any 'summit lesion'. Differential Diagnosis: In case of early 'summit lesion' in Pseudomembranous colitis one should rule out non-specific erosions due to local mucosal damage or early ulceration noted in some inflammatory disease processes. In ulcerative colitis there is glandular distortion and goblet cell depletion. It is sometimes difficult to distinguish advanced cases of PMC from ischaemic bowel disease. (In ischaemic colitis the mucosa is frankly haemorrhagic or show signs of glandular loss and fibrosis).
|
|
|

