|
|
|
Infectious Disease Online Pathology of Pinta
|
|
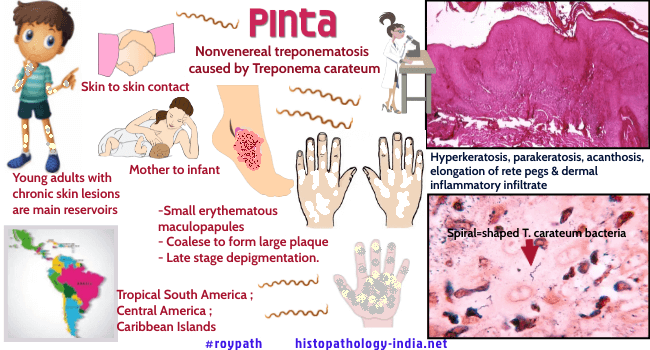
Pinta is a contagious, mild, systemic, nonvenereal treponematosis caused by Treponema carateum, which is morphologically identical to Treponema pallidum. Pinta is also known as mal de pinto (in Mexico and Cuba), enfermedad azul (blue illness, in Chile and Peru), and carate or cute (in Venezuela and Colombia). The disease occurs in the Central America and parts of remote, arid inland regions and river valleys of the tropical South America and various Caribbean Islands. Mode of transmission: Exact mode of transmission is not known. It is probably transmitted by direct skin to skin contact. Young adults (15 years old) with chronic skin lesions are considered to be the disease’s main reservoir. Pinta also appears to be transmitted to infants from their mothers by close contact. Clinical presentation: The lesions of pinta are confined to the skin and become very extensive. These are usually located on the extremities. The face, neck, chest and abdomen may also be affected. There is often overlap between the three clinical stages. Initial lesions are erythematous maculopapules, which grow by peripheral extension and often coalesce to form large plaques Papules are often itchy (pruritic). In some cases, nearby lymph nodes may be inflamed (lymphadenitis). One month to one year after the development of initial lesions, affected individuals may develop secondary skin eruptions called pintids. Pintids are small scaly, reddish lesions that normally affect the same sites as primary lesions. They may be dry and crusted (psoriatic pintids). The secondary lesions are widespread, long-lasting scaly plaques that show a striking variety of colours - red, pink, slate blue and purple. Pintids may recur for up to 10 years. The late phase of pinta occurs approximately two to five years after the development of initial lesions. These lesions merge with the late stage, in which depigmentation resembling vitiligo occurs, and sometimes there is epidermal atrophy.During this phase, affected individuals may also develop unusually dry, thickened skin on the soles of the feet and palms of the hands (hyperkeratotic). Eventually, affected individuals may develop dry,wrinkled thin (atrophic) skin in certain areas. Microscopic features: Primary and secondary lesions are identical and show hyperkeratosis, parakeratosis and acanthosis. There is exocytosis of inflammatory cells, sometimes with intraepidermal abscesses. Hypochromic areas show loss of basal pigmentation with numerous melanophages in the upper dermis. The dermal infiltrate, like the other changes, is heavier in established than in early lesions and includes lymphocytes, plasma cells and sometimes neutrophils. The infiltrate is predominantly superficial and perivascular. The treponemes can be demonstrated by silver methods - they are present mainly in the upper epidermis and are rarely found in the dermis. Darkfield examination of exudate and serologic tests for syphilis are positive when the secondary lesions appear. A single dose of long-acting penicillin is curative.
|
|
|
Copyright © 2022 histopathology-india.net

