|

Custom Search
|
|
Infectious Disease Online Pathology of Schistosomiasis
|
|
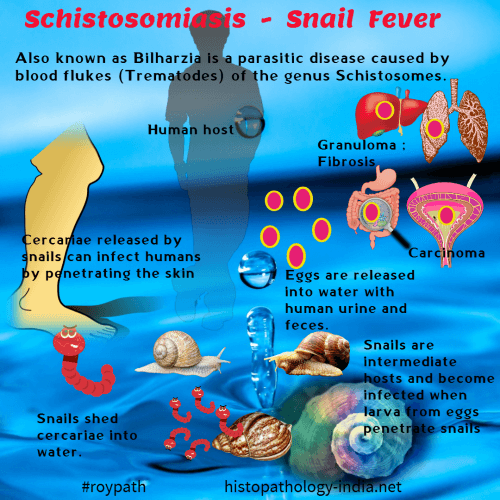
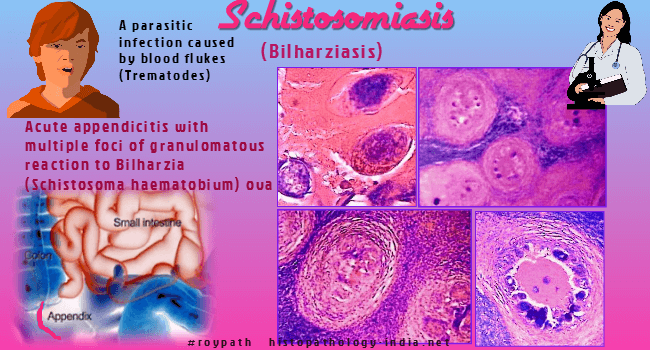
Schistosomiasis (bilharziasis) is a parasitic infection caused by blood flukes (Trematodes). Three main species cause human infection: 1.Schistosoma haematobium; 2.Schistosoma mansoni ; 3.Schistosoma japonicum. Epidemiology: DNA studies of Egyptian mummies shows evidence of the existence of Schistosomiasis about 5000 years ago. Schistosomiasis is increasing in prevalence, affecting nearly 10% of the world’s population and ranking second only to malaria as a cause of morbidity & mortality. Schistosoma haematobium are found in tropical Africa & part of southwest Asia. Schistosoma mansoni are found in tropical Africa, part of southwest Asia, south America & Caribbean islands. Schistosoma japonicum are found in parts of Japan, China, Philippines, India & part of southeast Asia. Blood flukes are known as schistosomes because of the "split body" on the ventral side of the male, in which the female is held during insemination and egg laying. Man is the definite host harbouring adult parasites, and fresh water snails are intermediate hosts.
Schistosoma mansoni: Clinical features: 1. Initially, at the site of entry of larvae, there is skin rash with pruritus, lasting for 1-2 days. 2. After 3-8 weeks of symptom-free period, there appear allergic manifestations, known as Katayama Syndrome, characterized by: i) Fever, chills, sweating, headache & cough. ; ii) Urticaria, muscle and abdominal pain and patches of pneumonia ; iii) Splenomegaly 3. Chronic cases : i) Portal hypertension with esophageal varices & hemorrhoids causing hemorrhagic manifestations. ii) Pulmonary hypertension causing cor-pulmonale iii ) Immune-complex Glomerulonephropathy iv) Transverse myelitis- due to involvement of spinal cord. Pathogenesis: Schistosomiasis has been referred to as an immunologic disease. The pathogenesis of acute and chronic schistosomiasis appears to involve immunologic mechanisms, either humoral or cell mediated. Delayed type of cell-mediated hypersensitivity is due to secretion of soluble enzyme by the ova. Delayed type of hypersensitivity helps ova to escape from intestinal blood capillaries into gut lumen. Schistosomes evade host immunity by covering its surface with host protein (red-cell glycoproteins, MHC molecule & IgG). It lives in mesenteric vessels of host, in spite of blood containing antibodies. It also develops two outer cytoplasmic lipid-layers, which are resistant to immune damage. Adult living schistosomes in veins provoke no inflammation. Dead worms become entangled as emboli to be arrested in liver or lung causing intense reaction. Pathology: Classic bilharzial granuloma: Basic lesion is a circumscribed granuloma consisting of a centrally located round ova together with epithelioid cells, fibroblasts, giant cells and some plasma cells and eosinophils. I. Skin lesion: Pruritic papular rashes. II. Intestinal Schistosomiasis: Distal rectosigmoid colon is most commonly involved. Ova are deposited in minute vessels of submucosa. Miracidia are released from ova by mechanical pressure & cytolytic enzymes, into gut lumen to be excreted in stool. If ova cannot be excreted through intestine it may be carried through portal vein to liver producing portal tract fibrosis. If ova are retained in the intestinal tissue, miracidia are disintegrated with fibrosis at the site. Mucosa of involved part shows granulation tissue with ova, causing polypoid hyperplasia of mucosa, which often bleeds and ulcerates. Ulcers with dense fibrosis cause narrowing of gut lumen. III. Hepatosplenic Schistosomiasis: Reticuloendothelial cell hyperplasia & granulomas are often seen in liver & spleen Liver : Ova lodged in the small intrahepatic portal radicles contain a living embryo that can survive for a period of 2-3 weeks. It secretes soluble antigen and induce granulomatous reaction. Intrahepatic portal radicle is totally replaced by a granuloma that occludes the lumen. Acute endophlebitis of the intrahepatic radicles may be noted. This may finally lead to intrahepatic vascular block. Inflammation and destruction of the coats of blood vessel lead to thrombosis. The thrombi become recanalized and the newly formed blood vessels communicate through the wall of the vein with adjacent vessels outside, forming telangiectasias in the portal area. Due to prominent vascular and fibrotic changes, the portal area is moderately broadened. Grossly liver is enlarged & slightly nodular. On cross section portal fibrosis stand out , termed as "pipestem" fibrosis. Intrahepatic portal fibrosis causes portal hypertension. Esophageal varices complicate the picture of portal hypertension. Death in patients with hepatosplenic involvement is usually due to rupture of these varices. Spleen: Enlarged with fibrosis & contain Gamma-Gandy bodies. IV. Cardiopulmonary lesion: For sufficient numbers of ova to reach the lungs, portal hypertension with collateral venous channels must be present to allow direct passage of eggs to the right-side of the heart and from there to the pulmonary arterial tree. Thus cardioovascular bilharziasis almost always occurs in patients with hepatosplenic schistosomiasis. There are granulomas around ova which may extend into the lumen of pulmonary vessels. Wall of the artery may be destroyed by the inflammatory process. Newly formed arteries in both intra-arterial & para-arterial granulomas , form anastomoses with pulmonary veins causing dilation of veins. Pulmonary obstructive arteriolitis causes pulmonary hypertension with right-sided heart Failure (cor-pulmonale). V. Immune complex Glomerulopathy of kidney: Majority of cases have histopathologic findings consistent with a diffuse membrano- proliferative glomerulonephritis. VI. Ectopic lesions: Solitary granulomas around ova may involve any organ or tissue, without any clinical effect. Solitary lesions are composed of numerous eggs, pseudotubercles, granulation tissue and varying amount of fibrous tissue. VII. CNS lesion: May affect brain causing symptoms of cerebral irritation and spinal cord causing transverse myelitis. Schistosoma Japonica: In human host the habitat of the organism is the lower mesenteric venous system. It may also be found in the veins of the small and large intestine. In general Schistosoma Japonica is characterized by similar but more serious symptoms than Schistosoma mansoni probably because of the larger number of eggs. Schistosoma japonicum produce similar lesions like Schistosoma mansoni except : 1) Involvement of small intestine is more frequent ; 2) Fibrotic and stenotic lesions of bowel are more common; 3) Intestinal polyps are more frequent; 4) Lesions in liver & lungs are more serious. Schistosoma Hematobium: Vesical and pelvic venous plexuses constitute the habitat of Schistosoma haematobium. In some cases the parasite may be retained in the haemorrhoidal plexus of veins or terminal tributaries of inferior mesenteric vein. Clinical features: i) Painless hematuria is the earliest symptom. ii) Other symptoms are, more or less, similar to Schistosoma mansoni. iii) Lesions in uterine cervix may simulate carcinoma of cervix. Pathological changes in Urinary bladder: Ova are deposited in submucosa of urinary bladder producing granulomas. Ova are excreted with urine. Mucosal changes are as follows: - Initial hyperemia and petechae ; - Polypoid or elevated areas covered with granular mucosa ; - Glandular hyperplasia (cystitis cystica) ; - Squamous metaplasia (leukoplakia); - Ulceration ; - Epithelium over calcified ova, appears as "sandy patch" at the base of bladder ; - Marked fibrosis around ureteric orifice causes bladder-neck obstruction with hydronephrosis and hydroureter. ; - Calcification may eventually occur. - In many patients carcinoma of the urinary bladder may develop. The disease may also affect the prostate, seminal vesicles, spermatic cord, epididymis, testes, penis, penile urethra and female urethra. Diagnosis: 1. Ova in stool, urine & tissue section. 2. Endoscopic findings of Intestine & urinary bladder. 3. Serodiagnosis: i) Indirect immunoflourescence. ii) Radioimmunoassay ; iii) ELISA. 4. Ultrasonography.
|
Further reading: Diagnosis and management of schistosomiasis Surgical pathology of schistosomiasis. Quantifying Quality of Life and Disability of Patients with Advanced Schistosomiasis Japonica |
|
|