|

Custom Search
|
|
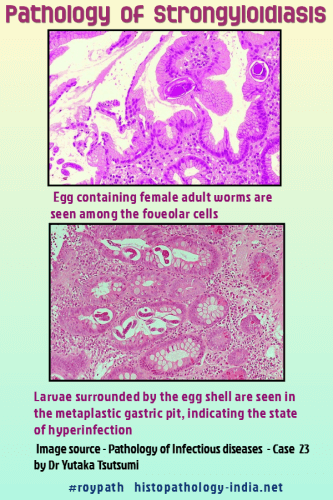
Infectious Disease Online Pathology of Strongyloidiasis
|
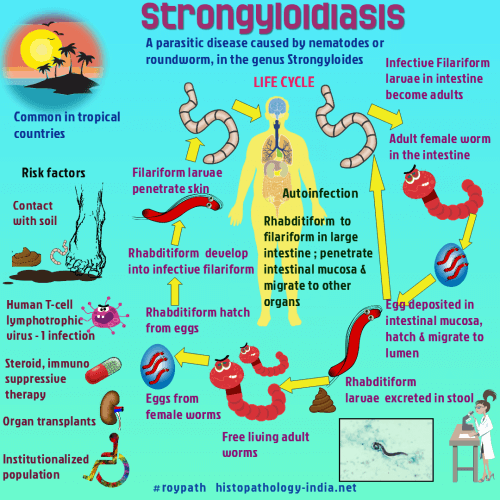
Strongyloidiasis, an infection by the nematode Strongyloides stercoralis, is encountered worldwide but is most common in tropical climates.In immunocompetent individuals Strongyloides stercoralis can produce asymptomatic infections or a moderate clinical picture of diarrhea, some cases become chronic. In immunocompromised patients, a disseminated disease may appear (strongyloides hyperinfection syndrome). This is a life threatening complication whereby larval proliferation leads to systemic sepsis and multiorgan failure.
Strongyloides stercoralis is a complex organism that has three life cycles.In one, parasitic parthenogenic females live in the human small intestine and lay eggs that hatch in the mucosal epithelium, releasing rhabditiform larvae.These larvae become infective within the intestine or on the perianal skin and invade human hosts directly (the autoinfection cycle).Alternatively, rhabditiform larvae pass in the faeces, become infective larvae in the soil, and later penetrate human skin (the direct development cycle).In the third possible cycle (the indirect development cycle), rhabditiform larvae passed in the faeces become free-living adults in the soil eventually produce infective larvae.These infective larvae penetrate the skin, enter blood vessels, and pass to the lungs, where they invade alveolar spaces.They ascend the trachea, descend the esophagus, and mature to become parthenogenetic females in the small intestine.Invading larvae cause transient dermatitis. Larvae migrating through the lungs may provoke cough, hemoptysis, and dyspnea, but most infections do not lead to pulmonary symptoms. Severe infection of the intestine is debilitating and causes vomiting, diarrhea, and constipation. This is often associated with the autoinfective cycle. In patients with suppressed immunity, infective larvae are more likely to penetrate the intestinal mucosa and invade the body. This "hyperinfection" strongyloidiasis may cause malabsorption and hypoproteinemia with anasarca, and may be severe enough to kill the patient. Obstruction from paralytic ileus and from thickening and immobility of the colon are characteristic of persistent hyperinfection. Female worms and rhabditiform larvae living in jejunal crypts cause mild eosinophilia and chronic inflammation. By contrast, patients with hyperinfection may have ulceration, edema, congestion, fibrosis, and severe inflammation of the intestine. In such cases, filariform larvae invade both the small and large intestine and may travel to any organ. Larvae in tissues may cause no reaction or may provoke microabscesses or granulomas. Adult T cell leukemia is often associated with strongyloidiasis. In tropical countries disseminated strongyloidiasis can be a fatal complication in AIDS patients. The diagnosis is made by identifying larvae in the stool. Larvae may occasionally be present in sputum, pleural effusions and urine. Chemotherapy is generally unsatisfactory, but thiabendazole may be useful.
|
|
|