|

Custom Search
|
|
Dermpath-India Pathology of Syringocystadenoma Papilliferum
|
|

Custom Search
|
|
Dermpath-India Pathology of Syringocystadenoma Papilliferum
|
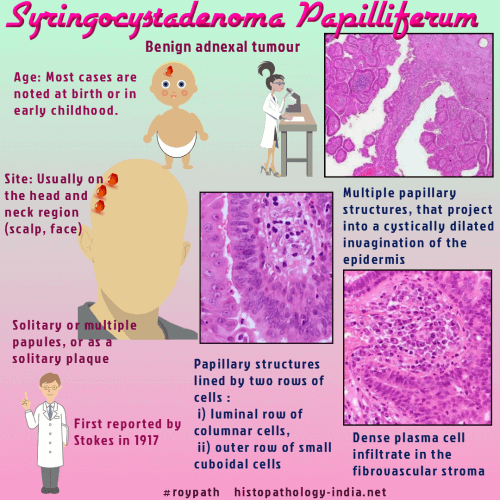
| Syringocystadenoma papilliferum
is an adnexal tumour which commonly occurs on the scalp, forehead
or face.
Rarely these tumours are found on the trunk, the lower extremities, ear canal and eyelid.
It was first described as
"nevus syringadenomatosus papilliferus" by Stokes in 1917. The results of light, electron microscopic, immunohistochemical and anatomic studies are conflicting. Many authors believe that syringocystadenoma papilliferum is mainly apocrine derived tumour because of the occasional presence of decapitation secretion in some of the luminal cells of the tumour and the frequent presence of tubular glands with large lumina and decapitation secretion beneath the tumour. In some lesions, where there are no apocrine glands in the dermis, the papilliferous structures represent eccrine proliferation. Most authors agree that this hamartoma develops from undifferentiated
pluripotential appendageal cells. Clinically, most of the cases are first noted at birth. Other cases develop in infancy, childhood and adolescence. The tumour presents either as one papule or several papules in a linear arrangement, or as a solitary plaque. Some papular lesion may be umbilicated and resemble molluscum contagiosum. During evolution of lesion verrucous changes can develop at puberty. The plaque type lesion is similar to nevus sebaceous.
Syringocystadenocarcinoma Papilliferum: Syringocystadenocarcinoma papilliferum is a distinct dermatologic entity. This exceedingly rare neoplasm, most examples of which seem to have arisen in its benign counterpart, syringocystadenoma papilliferum. Histologically, this malignant tumour shows in-situ adenocarcinoma with cytological atypia and pagetoid spread into surrounding epithelia. The tumour lacks typical double layered pattern. Decapitation secretion is present. Immunohistochemistry shows immunoreactivity to EMA and human milk fat globules.
|
|
Further reading: Syringocystadenoma papilliferum arising on the scrotum. Syringocystadenoma papilliferum: an unusual cutaneous lesion in a pediatric patient.
|
|
|
Visit:- Infectious Disease Online
Copyright © 2022 histopathology-india.net