|

Custom Search
|
|
Infectious Disease Online Pathology of Toxoplasmosis
|
Toxoplasmosis is caused by the obligate intracellular protozoan Toxoplasma gondii. The parasite was originally identified in the small North African rodent Ctenodactylus gundi, hence its name. "Toxo"- refers to the curved or arcuate shape of the organism, not to a toxin. It is widely distributed among domestic animals and humans throughout the world. Toxoplasma is a tissue coccidium. Both coccidian stages, schizogonic and gametogonic, are found in the epithelium of the small intestine of cats. The toxoplasma oocyst, similar in morphology to that of Isospora belli , is excreted in cat faeces. The oocyst , millions of which may be shed in a single stool of an infected cat, survive for months in moist environments, water or soil.
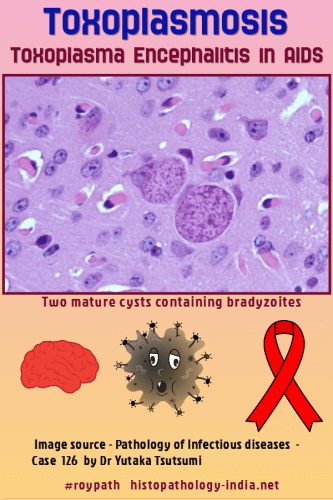
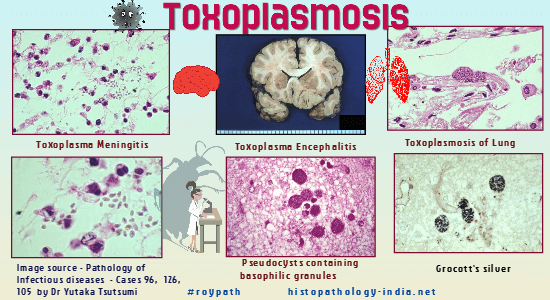
In human tissues proliferating tachyzoites (trophozoites) and cysts may be identified. The presence of tachyzoites is diagnostic of acute infection. Cysts containing hundreds and sometimes thousands of bradyzoites make their appearance in brain, skeletal muscles, and other tissues with the development of immunity. Rupture of these cysts has been proposed as a pathogenetic mechanisms for the development of inflammatory lesions. Toxoplasma tachyzoites enter the cells by both phagocytosis and active invasion. The latter mode of entry depends on specialized organelles, called rhoptries, and on "penetration-enhancing factor." During this infectious process an oxidative respiratory burst is not stimulated, thus no oxygen metabolites are formed to kill the protozoan. T. gondii also alters the membrane of the parasitophorous vacuole so that lysosomal fusion does not take place. Mode of infection: - Oocysts and cysts are the principal infective forms. Infection occurs when a person eats undercooked or raw meat of animals with chronic toxoplasmosis or ingests oocysts from the faeces of cats. - Recently an outbreak of acute toxoplasmosis associated with ingestion of contaminated water was reported. Most of these primary infections are asymptomatic and result in a chronic carrier stage. These cases are mostly symptomless. - Transplacental transmission occurs rarely but accounts for the majority of patients. Infection of the fetus is seen in 30% to 40% of cases of acquired toxoplasmosis during pregnancy. Relatively few cases of human disease have been reported in immuno-competent hosts, but results of the skin test for toxoplasma have been positive in 10% to 50% of the adults tested, indicating that although disease is rare infection is common. The prevalence of the disease can be less than 10% in dry areas (Example: Arizona) and close to 100% in moist lowland tropical areas (Example: Costa Rica and Guatemala). Prevalence increases with age. The majority of immunocompetent individuals infected with Toxoplasma have minimal or no symptoms. However, in immunocompromised patients disseminated disease can occur and it is often fatal. Central nervous system toxoplasmosis is the major form of involvement in these patients. Patients with the acquired immunodeficiency syndrome (AIDS) frequently develop neurologic manifestations resulting from toxoplasmic encephalitis or brain abscess, or both. Toxoplasmosis in Pregnancy: Pregnant women who acquire infection from Toxoplasma gondii usually remain asymptomatic, although they can still transmit the infection to their fetuses with severe consequences. Given the asymptomatic nature of most Toxoplasma infections, primary prevention in pregnant women may lower the risk of congenital toxoplasmosis. Both consumption of undercooked meat and unprotected contact with soil are independent risk factors for T. gondii seroconversion during pregnancy, while contact with cat litter may pose a risk in certain situations. The clinicopathologic presentation in toxoplasmosis varies according to the age and the immune status of the patient. The three distinct presentations are as follows: (1) Congenital Toxoplasmosis in neonates: Congenital or neonatal toxoplasmosis should be strongly suspected when the characteristic ocular lesions and the presence of cerebral calcifications in radiological examinations are associated with hydrocephalus and pleocytosis of the cerebrospinal fluid. The pathologic lesions are those of hydrocephalus caused by necrotic foci in the brain, usually located in the periventricular areas. These lesions are microglial nodules surrounded by areas of vasculitis and necrosis. Calcium deposits in these focal lesions and bilateral chorioretinitis are evident. Focal areas of necrosis may be seen in viscera, leading to myocarditis, pneumonitis and rarely hepatitis. (2) Toxoplasma Lymphadenitis in immunocompetent adults: The clinical picture of adult toxoplasmosis is uncommon. It consists in lymphadenitis (usually posterior cervical), fever and malaise. A biopsy of the firm, rubbery nodes is commonly done to rule out lymphoproliferative diseases, and it is the pathologist who first suggests the diagnosis of toxoplasmosis. The architecture of the lymph node is preserved. There is pronounced follicular hyperplasia, sinus histiocytosis and clusters of epithelioid histiocytes inside and surrounding the follicles. Specificity of the histopathological triad for the diagnosis of toxoplasmic lymphadenitis: polymerase chain reaction study. Organisms are rarely seen. Pathologic diagnosis can be confirmed serologic methods such as indirect immunofluorescence, indirect hemagglutination, complement fixation, and enzyme-linked immunosorbent assay. Some of these serologic tests have been suggested as screening methods for toxoplasmosis in pregnancy. Acute infection is diagnosed on the basis of a fourfold rise in antibody titre or detection of IgM antibodies by the indirect immunofluorescence method. A Paul-Bunell test for heterophil antibodies is usually done to rule out infectious mononucleosis. (3) Toxoplasma Encephalitis in Immunocompromised Host: Well circumscribed areas of hemorrhage and necrosis are frequently identified by CT scan and on gross inspection. Microscopic examination usually reveals necrosis, vascular thrombosis, and the presence of tachyzoites. Immunoperoxidase and immunofluorescence methods have recently been developed for the diagnosis of toxoplasmosis in tissue sections. Other, less common manifestations of toxoplasmosis are interstitial pneumonitis , myocarditis and hepatitis. Chorioretinitis and uveitis sometimes occur. The most effective treatment for toxoplasmosis consists of sulfadiazine and pyrimethamine.
|
|
What is Sabin-Feldman
dye test? This test is based on the observation that live tachyzoites stain blue with alkaline methylene blue dye. Live tachyzoites are mixed with different dilutions of the patient's serum and the mixtures are then incubated for an hour, stained with dye, and examined with a microscope. If antibodies to T gondii are present in the patient's serum, they will damage the organisms. The damaged organisms will not take up the dye and appear as pale "ghosts" compared to undamaged organisms. The test requires live tachyzoites and is difficult to perform, so other serological tests are typically used. However, the test is very sensitive and specific.
|
|
Further reading: Photographs related to Pathology of Toxoplasmosis Chronological Development of Cellular Immunity in Human Toxoplasmosis |
|
|
Copyright © 2022 histopathology-india.net