|

Custom Search
|
|
Infectious Disease Online Pathology of Trachoma
|
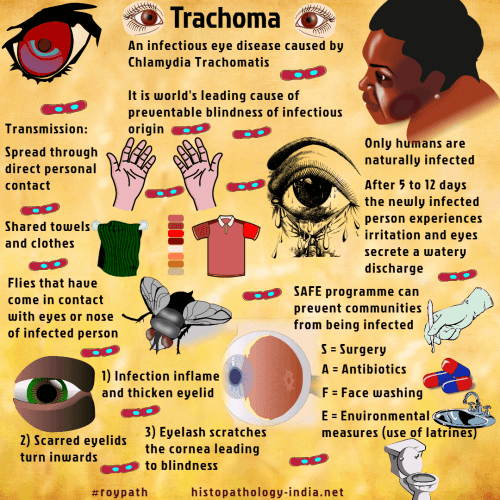
Trachoma is a chronic progressive infection of the conjunctiva and cornea that may cause partial or total blindness. Infection with Chlamydia trachomatis, subgroups A, B, Ba, and C is the leading cause of preventable blindness in the world. The blinding complications are associated with progressive conjunctival scarring. The disease is worldwide, associated with poverty, and most prevalent in dry or sandy regions. Only humans are naturally infected. Poor personal hygiene and inadequate public sanitation are common factors. Mode of infection: Spread mostly by direct contact, trachoma is also transmitted by fomites, contaminated water, cosmetics, and probably flies. Subclinical infections are an important reservoir. Clinical presentation: In endemic areas infection is acquired early in childhood, becomes chronic, and eventually progresses to blindness. An abrupt onset of palpebral and conjunctiva inflammation leads to lacrimation, purulent conjunctivitis, and photophobias. As chronic inflammation progresses over months and years there is scarring of the upper tarsal plate and corneal keratitis, with formation of a vascular pannus. Scarring, trichiasis and entropian eventually interfere with normal ocular function. Secondary bacterial infections and corneal ulceration are common.
Diagnosis of Trachoma: Diagnosis of trachoma is based on the clinical findings and the demonstration of organisms in smears or cultures. Scrapings of the superficial conjunctiva stained with Giemsa or by direct immunofluorescence may reveal diagnostic intracytoplasmic inclusions. Treatment: Trachoma responds to topical and systemic tetracycline, but endemic trachoma is difficult to treat because of repeated exposure. All members of a family or social group should be treated to prevent retransmission. Vaccines have been ineffective, and those administered systemically tend to exacerbate the disease. Improved hygiene and public sanitation are the most effective control measures.
|
|
|
Copyright © 2022 histopathology-india.net

