|

Custom Search
|
|
Infectious Disease Online
Pathology of Whooping Cough (Pertussis)
|
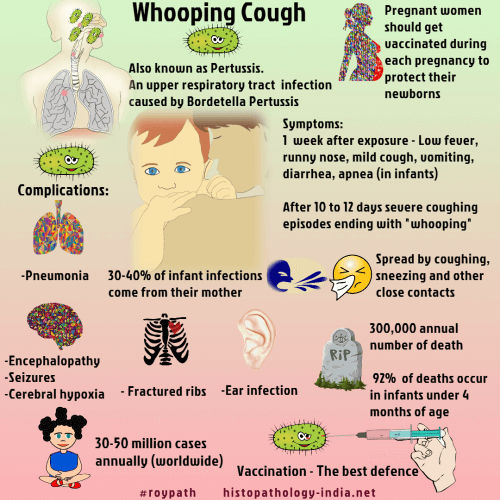
Whooping cough is caused by Bordetella pertussis, a nonmotile, gram-negative coccobacillus that forms a capsule in its virulent state. Humans provide the only reservoir. Bordetella pertussis produces a heat-labile toxin, a heat-stable endotoxin, and a lymphocytosis-producing factor also called histamine-sensitizing factor. Pertussis is a worldwide problem and passes from person to person in moist droplets containing Bordetella pertussis. Nearly all susceptible contacts become infected. Bordetella pertussis has a remarkable ability, probably enhanced by its pili, to attach to ciliated bronchial epithelium. Here the organisms proliferate, remain on the surface epithelium and accumulate in great numbers. The bacteria stimulate the bronchial cells to produce a profuse, tenacious mucus that slows ciliary action and inhibits the bronchopulmonary toilet. Secondary bacterial infections and epithelial necrosis follow. A catarrhal stage begins 7 to 10 day after exposure and may last 1 to 2 weeks. There is low-grade fever, rhinorrhea and conjunctivitis. During the catarrhal stage, when the patient is most infectious, B. pertussis proliferates, forms entangled masses mixed with the cilia, and elicits a neutrophilic exudate. Cough progresses to severe paroxysms terminating in a gasping, strident, inspiratory effort. During inspiration, air is forcibly drawn through a narrow glottis, giving the characterisitic "whoop". This paroxysmal stage begins 2 - 3 weeks after inoculation, lasts days to weeks and is marked by as many as 50 paroxysms per day. The necrotic bronchial epithelium is covered by a thick mucopurulent exudate. The convalescent stage lasts weeks or (rarely) months. The death rate is highest in infancy. B.pertussis infections in infancy are frequently associated with apneic spells, which are occasionally life-threatening and, if leading to death, might be reported as Sudden Infant Death Syndrome (SIDS). Immunity is conferred by IgA antibody, which prevents bacterial attachment. Second attacks can occur but are caused by Bordetella parapertussis which may cause 20% of all whooping cough infections. Vaccination protects against Bordetella pertussis , but not against B. parapertussis. Morphological findings: Morphologic changes, in the uncomplicated case, are mostly limited to the air passages and lung. Findings include laryngitis, tracheitis, bronchitis and the bronchiolitis . The changes are most noticeable in the bronchi. Bacterial stains reveal many of the specific organisms contained within the mucopurulent exudate that overlies the mucosa and is intertwined and tangled with the cilia of the columnar epithelium. Occasionally, areas of superficial necrosis and erosion are evident. Hyperemia and excessive production of mucus occur. The smaller bronchi may contain dense plugs of mucus and these will include a few inflammatory cells and many organisms. Peribronchitis and interstitial pneumonitis , especially around small bronchi are characterisitic findings but are not pathognomonic, since they are seen also in other disease. Little exudate is to be found in alveoli unless there is secondary bronchopneumonia. Emphysema is almost always evident microscopically. Peribronchial lymph nodes are hyperemic and exhibit moderate hyperplasia. B. pertussis may be cultured from the posterior nasopharynx during the first 2 weeks. Smears from nasopharyngeal swabs can be tested with fluorescent-labeled antipertussis serum. A combination of culture and fluorescent-labeled smears gives the greatest diagnostic accuracy. Erythromycin is effective in the catarrhal stage and should be given to all contacts with positive nasopharyngeal smears. Antibiotics begun after the paroxysmal stage begins do not alter the clinical course.
|
Further reading: Bordetella pertussis infection attenuates clinical course of acute bronchiolitis. |
|
|
Copyright © 2022 histopathology-india.net

