|

Custom Search
|
|
Infectious Disease Online Pathology of Anisakiasis
|
|
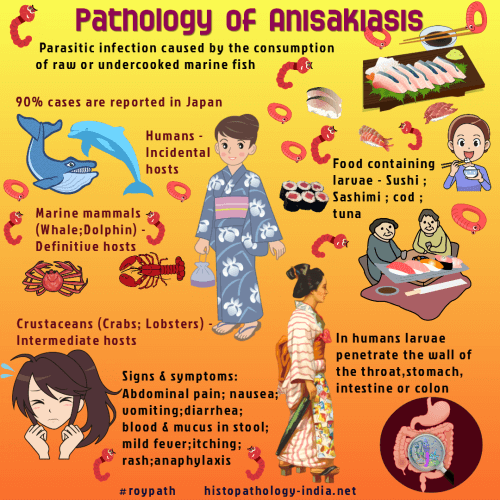
Anisakiasis is a parasitic infection caused by the consumption of raw or undercooked wild marine fish infected with larval nematodes belonging to the genus Anisakis (Anisakis simplex, Anisakis pegreffii and Pseudoterranova decipiens) . The first case of anisakiasis, was reported by van Thiel et al. in 1960. [ Note: Anisakiasis caused by Anisakis simplex - Herringworm disease ; Whaleworm disease. Anisakiasis caused by Pseudoterranova decipiens - Codworm disease; Sealworm disease.] Every year, approximately 20,000 anisakiasis cases are reported worldwide. More than 90% of these cases are from Japan, most others occur in Spain, Netherlands, and Germany, depending on the habits of raw fish consumption. Aniskiasis is contracted when inadequately cooked fish containing these nematode larvae are eaten. Popular foods containing viable larvae are pickled herring in Scandinavian countries, sushi or sashimi in Japan, and cod, flounder, and tuna from the east coast of the United States. Nematodes causing anisakiasis have a marine mammal (whale, dolphin) as the definitive host. Note: Crustaceans are the first intermediary hosts. Various species of fish and some cuttlefish are second intermediary hosts. Humans are only accidentally infected. In humans the larvae penetrate the wall of the esophagus, stomach, intestine or colon. Intestinal discomfort begins a few hours after eating the fish. Larvae are released from the muscle of the fish, penetrate the gastric or intestinal mucosa, or become attached in the throat without invasion of tissue.
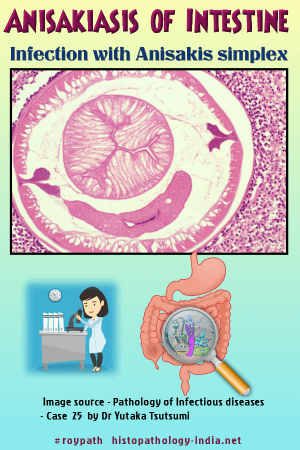
Surgical case of intestinal anisakiasis provoking eosinophilic cellulitis.The Anisakis larva is histologically characterized by a pair of clover-shaped lateral chords, eosinophilic Renett cells (exocretory organ), and the gut consisting of high columnar cells.
Note: Anisakiasis is classified as either the luminal or the invasive form, according to the presence of bowel wall invasion by Anisakis larvae. The luminal form does not cause major clinical symptoms, but the invasive form can. The invasive form is subdivided into gastric and intestinal types, according to the penetration site. Cases of gastric anisakiasis (95%) are more common than are those of enteric anisakiasis, and the latter is rarely reported. Infection is diagnosed after surgical intervention for intestinal obstruction or peritonitis, which is caused by necrotizing, eosinophilic, granulomatous inflammation. Worms in the throat or stomach are frequently vomited or coughed up, and a common clinical presentation is a wriggling sensation in the throat, with larvae appearing in the mouth of an alarmed patient. Intestinal anisakiasis clinically resembles appendicitis, with right lower quadrant pain, nausea, and vomiting. Continued migration to omentum or mesentery is common. Worms lodge in and thicken the gastric or bowel wall. The identification of larvae provides the diagnosis. Infections of the small intestine, caecum, or colon are usually not diagnosed before exploratory laparotomy. Removal of worms relieves the symptoms. This parasitic infection should be considered in the differential diagnosis of acute abdominal syndromes and eosinophilic infiltrates of the stomach, small intestine, colon, omentum, and mesentery, especially with a history of raw marine fish consumption.
|
| Further reading: |
|
|
Copyright © 2022 histopathology-india.net