|

Custom Search
|
|
Infectious Disease Online Pathology of Balantidiasis (Balantidium Coli)
|
|
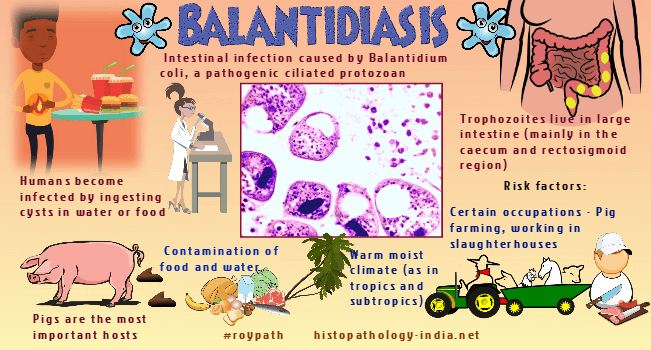
Balantidiasis, infection by the protozoan Balantidium coli, is encountered worldwide, but infections are more common in tropical and subtropical regions. Balantidium coli infects many animals but pigs and rats are the most important reservoirs. Balanatidiosis should be included in the differential diagnosis for persistent diarrhea in travelers to or from Southeast Asia, the Western Pacific islands, rural South America, or communities where close contact with domestic swine occurs. In some developing countries and rural areas where pig and human fecal matter contaminates the water supply, there is a greater chance that balantidiosis may develop in humans. Balantidium coli is a ciliated protozoan with two stages - cyst and trophozoites.In tissue sections, the trophozoites usually measures 25-40 x 40-80 micrometer.The trophozoites are oval, with a slightly pointed anterior end and a rounded posterior end.The thin cell membrane is ciliated.The foamy cytoplasm contains vacuoles, a large macronucleus and a small micronucleus.Cysts are round or oval, 40 to 65 micrometer across, and have both a micro and a macronucleus.Trophozoites of Balantidium coli live in the large intestine and are concentrated in the caecal and sigmoidorectal regions. They multiply by transverse biniary fission and under some conditions transform into cysts that are passed in the stool. Humans become infected by ingesting cysts in water or food. After ingestion, the cyst wall dissolves and liberates trophozoites that invade the mucosa of the large intestine. Most balantidial infections are asymptomatic or characterized by intermittent diarrhea or constipation. Severe infections may cause abdominal pain, colonic tenderness, fever, anorexia, and severe diarrhea. Other symptoms are headache, insomnia, nausea, vomiting, cachexia, pallor, weakness, anemia, dehydration, malaise, and distention. Stool specimens may be watery and contain blood, mucus, and pus. Balantidia invade the bowel wall and cause ulcers that resemble amebic ulcers. The ulcers are flask-shaped with undermined edges and may involve the entire thickness of the intestine. The base of the ulcer is formed by a zone of coagulative necrosis that contains balantidial trophozoites. Beyond the necrotic bed the tissues are edematous and contain chronic inflammatory cells, mostly lymphocytes and plasma cells. Rarely, an ulcer may perforate the bowel wall. Diagnosis is usually made by identifying trophozoites or cysts of Balantidium coli in the stool or in a biopsy specimen taken through a sigmoidoscope, or by finding trophozoites in the ulcer at autopsy. Effective sanitation and uncontaminated water are the most useful weapons against infection. Tetracycline or iodoquinal are treatment of choice.
|
|
|
Visit:- Dermatopathology Online
Copyright © 2022 histopathology-india.net

