|

Custom Search
|
|
Infectious Disease Online Pathology of Mycoplasma Pneumoniae Pneumonia
|
|
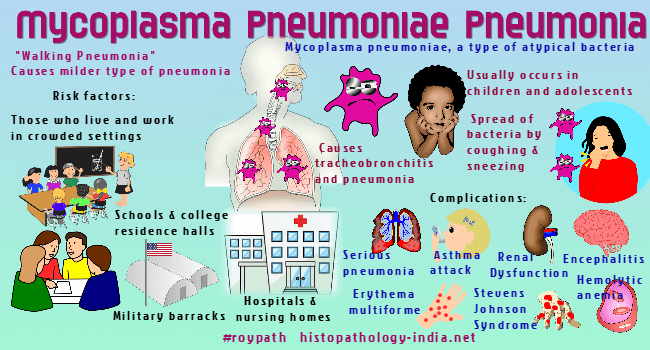
Mycoplasma pneumoniae causes tracheobronchitis and pneumonia, most frequently in children and adolescents. It is a milder type of pneumonia and is also known as "walking pneumonia". Infections are world wide and account for about 20% of all cases of pneumonia in some cities. Most infections occur in small groups of people who have frequent close contact, for example, families, military units, and closed institutions. The organism is spread by aerosol transmission from person to person over a period of several months, with an attack rate of greater than 50% within the group. The incubation period is 2 to 3 weeks, and the onset is insidious. Clinical features are an initial nonproductive cough followed by the production of watery or mucoid sputum, fever, rhinorrhea, chest pain, and generalized myalgia. The diagnosis is made by culturing Mycoplasma pneumoniae in special cell-free media after inoculating specimens of sputum, throat swab, pleural fluids, or tissues. Infections commonly involve the oropharynx, trachea, bronchi, and lungs, usually causing unilateral pneumonia of the lower lobe. The radiographic appearance cannot be distinguished from that of other nonbacterial pneumonias. The infection is superficial, with the organisms attaching to ciliated epithelial cells. Electron microscopy reveals that the mycoplasma has a specialized tapered, filamentous tip with a rodlike core, which may attach the mycoplasma to the epithelial cell. Mycoplasma pneumoniae does not produce endotoxin or exotoxin but does produce hydrogen peroxide and superoxide (O2-). Microscopically, there is a patchy interstitial pneumonia with swollen alveolar lining cells, bronchiolar walls thickened by congestion and edema and an intraluminal exudate of neutrophils, epithelial cells, and proteinaceous debris. The initial infiltrate, predominantly a perivascular and peribronchial cuffing by lymphocytes and macrophages. The pulmonary changes are often complicated by bacterial superinfection. In rare instances other organs may be involved (central nervous system, pancreas, joints, skin, heart, and pericardium), probably as a result of hematogenous spread. The diagnosis of infection with Mycoplasma pneumoniae is made by detecting specific compliment-fixing antibodies. The symptoms and signs of mycoplasma pneumonia usually abate within 10 to 14 days, and recovery is hastened by treatment with broad-spectrum antibiotics. Patients continue to shed mycoplasmas for some times after therapy has been discontinued but usually recover without sequelae. Complications include: Serious pneumonia ;Asthma attacks or new asthma symptoms ; Encephalitis (swelling of the brain) ; Hemolytic anemia ; Renal dysfunction ; Skin disorders (Stevens-Johnson syndrome, erythema multiforme, toxic epidermal necrolysis).
|
|
|
Copyright © 2022 histopathology-india.net

