|

Custom Search
|
|
Infectious Disease Online Pathology of Necrotizing Fasciitis (Flesh Eating Disease)
|
|

Custom Search
|
|
Infectious Disease Online Pathology of Necrotizing Fasciitis (Flesh Eating Disease)
|
|
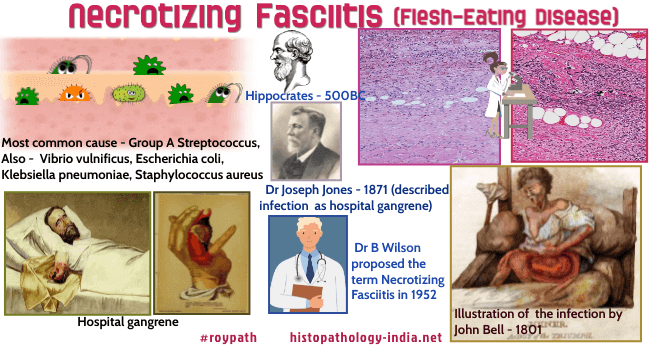
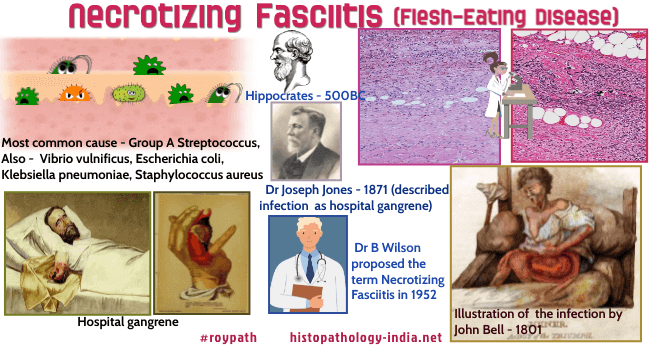
Syn: hemolytic streptococcal
gangrene, Meleney ulcer, acute dermal gangrene, hospital gangrene,
suppurative fasciitis, and synergistic necrotizing cellulitis. Necrotizing soft tissue infection was first described in 500BC by Hippocrates. In 1871, Dr Joseph Jones, an American army surgeon during the American Civil War, described this infection as hospital gangrene. In 1952, Dr B.Wilson proposed the term of necrotizing fasciitis and included both gas forming and nongas forming necrotizing infections. Necrotizing fasciitis is commonly known as "flesh-eating disease". The deep-seated infection of the subcutaneous tissue causes rapid destruction of fascia and fat and can eventually lead to death of the patient Necrotizing fasciitis is classified into broadly into two types, Polymicrobial and Monomicrbial. Type I NF refers to mixed infections (Polymicrobial) involving anaerobes (Bacteroides and Peptostreptococcis species), and one or more facultative anaerobes, such as streptococci (non-group A β-hemolytic Streptococcus) and members of the Enterobacteriaceae family (eg, Escherichia coli, and Enterobacter, Klebsiella and Proteus species). Type II NF (Monomicrbial) refers to infections that are caused by invasive group A β-hemolytic Streptococcus. Type II can also be caused by S. aureus, Vibrio vulnificus, Aeromonas hydrophila, and various fungi such as Mucor, Rhizopus, or Rhizomucor. Necrotizing fasciitis can occur in soft tissues, but most common areas of expansion are the extremities, (particularly the lower legs) where it commences as a poorly defined erythema,serosanguineous blisters develop and subsequently necrosis occurs at the centre. Trunk, abdomen, head, neck area, or anal region are also often infected after surgery. Lesions on the perineum and genital area with possible infection of the abdominal wall are called "Fournier's gangrene". Common triggers are trivial trauma, burns, surgery, decubital ulcers, perirectal abscesses or Fournier's gangrene and risk factors include diabetes mellitus, immunosuppression, malnutrition, age, intravenous drug misuse, peripheral vascular disease, renal failure, malignancy, and obesity. Patients with necrotizing fasciitis usually present with severe pain around the affected area and signs of skin infection (erythema, swelling, oedema, subcutaneous plaques, or surface nodes). These physical findings may rapidly evolve into a haemorrhagic infarction of the subcutis, the fascia and the dermis with the formation of painless gangrene. Microbial invasion of the soft tissues occurs either through external wound from trauma or direct spread from injured hollow viscus (particularly the lower gastrointestinal tract including the colon and rectum) or genitourinary organs. Microbial growth within the soft tissues releases a mixture of cytokines and endotoxins/exotoxins, causing the spread of infection through the superficial and deep fascia. This process causes poor microcirculation and ischemia in affected tissues, ultimately leading to cell death and tissue necrosis. The death rate may be as high as 30%–70% with death being due to sepsis, respiratory failure, kidney failure, or multiorgan system failure. Mortality rate is higher in women over 60 years of age, having chronic heart disease, liver cirrhosis, skin necrosis, pulse rate >130/min, systolic blood pressure <90 mmHg, and serum creatinine level ≥1.6 mg/dL. Necrotizing fasciitis is a serious infection of skin and soft tissues that rapidly progresses along the deep fascia. It becomes a fatal soft tissue infection with high death rate if treatment is delayed. Early diagnosis for emergency surgical debridement and broad-spectrum antibiotic therapy are necessary treatments to reduce death rate in this deadly infectious disease. Visit: Vibrio Vulnificus ;
|
|
Source Descamps V, Aitken J, Lee MG. Hippocrates on necrotising fasciitis. Lancet. 1994;344:556 Jones J. Surgical memoirs of the war of the rebellion: investigation upon the nature, causes and treatment of hospital gangrene as prevailed in the Confederate armies 1861-1865. New York: US Sanitary Commission; 1871. Wilson B. Necrotizing fasciitis. Am Surg. 1952;18(4):416–431. Koch C, Hecker A, Grau V, Padberg W, Wolff M, Henrich M. Intravenous immunoglobulin in necrotizing fasciitis – A case report and review of recent literature. Annals of Medicine and Surgery. 2015;4(3):260-263.
|
|
|
Copyright © 2022 histopathology-india.net