|

Custom Search
|
|
Infectious Disease Online Pathology of Trichosporonosis
|
|
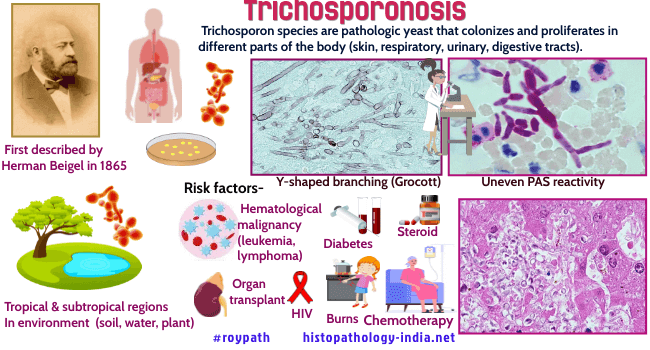
The Trichosporon species have recently emerged as significant systemic pathogens in immunocompromised patients. Hermann Beigel first described the genus Trichosporon in 1865 upon discovering that it can cause a benign hair shaft infection. These yeast-like fungi are soil saprophytes that also form a minor component of normal skin flora. The classification and naming of Trichosporon has then changed multiple times over the years. Initially, all Trichosporon spp. were classified as Trichosporon beigelii, and it was thought that the strain mainly causes infection in superficial hair, and rarely causes deep-seated infection. However, subsequent research showed that T. beigelii has great morphologic variation, as well as physiological and biochemical variance. In 1992, Gueho et al. revised the taxonomy of 20 species of Trichosporon, including six pathogens: Trichosporon asahii, T. asteroides, T. cutaneum, T. inkin, T. mucoides and T. ovoides. Almost all cases of Trichosporon infection reported before 1994 were named T. beigelii. In contrast, isolates of Trichosporon spp. reported in the past 20 years are of various types, and numerous species of Trichosporon are known to exhibit different pathogenic characteristics. For example: 1) T. asteroids and T. cutaneum are the main pathogenic species known to cause superficial skin infections. 2) T. asahii is the most prominent clinical pathogen, better known as the agent of white piedra, a nodule-forming trichomycosis. 3)Trichosporon ovoides - White piedra (scalp hair) ; Trichosporon inkin - White piedra (pubic hair) 4)Trichosporon mucoides (Systemic trichosporonosis) Disseminated trichosporonosis occurs principally in patients who are neutropenic as a result of treatment for acute leukemia, lymphoma, or solid tumours but it has also been reported in immunosuppressed transplant recipients. Purpuric cutaneous nodules are a frequent clinical manifestation, and the lungs, kidneys, myocardium, liver, spleen, and bone marrow are also frequently involved. Systemic lesions consist of abscesses, granulomas, or nodular infarcts, the last a consequence of mycotic vascular invasion and occlusion. In tissue sections, the Trichosporon spp can be recognized as pleomorphic blastoconidia , 3 to 8 micrometer in diameter, septate hyphae, and arthroconidia that are produced by fragmentation of hyphal segments. These fungi may be difficult to distinguish from some other opportunistic pathogen, such as the Candida species, if arthroconidia are inconspicuous. A presumptive histologic diagnosis of trichosporonosis is therefore best confirmed by culture or immunoflourescence.
|
|
|
Copyright © 2022 histopathology-india.net

