|

Custom Search
|
|
Infectious Disease Online Pathology of Rocky Mountain Spotted Fever
|
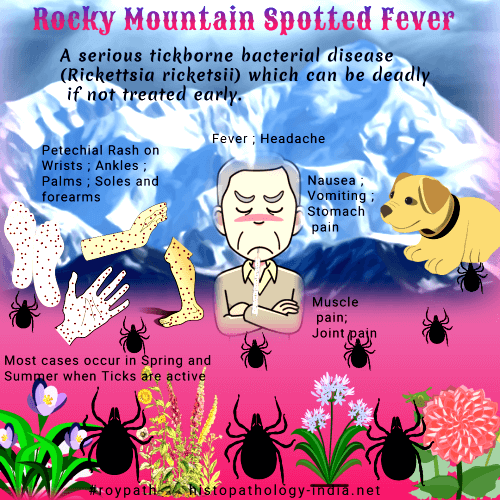
Rocky Mountain spotted fever is one of the severest infectious disease, with a mortality in previously healthy persons of 20% before the advent of antimicrobial therapy.Rocky Mountain spotted fever is the most important rickettsiosis in the United States from the aspects of morbidity and mortality.Most cases occur in the spring and summer when the ticks are active.However, contrary to its name, cases occur throughout the U.S.A. as well as in Central and South America with the majority of cases occurring in the Southeastern states. ArticleRickettsia rickettsii are released from the salivary glands of a feeding Dermacentor variabilis, Dermacentor andersoni, Rhipicephalus sanguineus, or Amblyomma cajennense tick and are injected into the feeding blood pool in the host’s skin.Clinical presentation: After an incubation period of 2 to 12 days the patient develops severe headache, fever, and frequently nausea, vomiting, or abdominal pain.A maculopapular rash appears on the wrists and ankles 2 to 5 days later, usually spreads to involve the trunk, palms, and may become petecheal.Delay or absence of rash and frequent lack of a history of tick bite make misdiagnosis and fatality a genuine problem.In severe cases the patient may manifest signs of encephalitis, noncardiogenic pulmonary edema, skin necrosis, coagulopathy with bleeding, acute renal failure failure, jaundice, hypovolemic shock.In fatal cases death usually ensues 8 to 15 days after onset of symptoms.There is a fulminant form of Rocky Mountain spotted fever, observed most often in glucose-6-phosphate dehydrogenase deficient black males in which the patient may die before the fifth day of illness.Early treatment with tetracycline or chloramphenicol cures most patients, however, late diagnosis and inappropriate treatment result in an overall mortality of 3% to 8%.
Pathogenesis: Thrombosis and activation of the kallikrein-kinin pathways may exacerbate the disease and the acute-phase response presumably mediated by interleukin-1 is observed. Rickettsia rickettsii does not seem to produce a toxin. Direct injury of infected cells by rickettsiae has been documented. The pathogenic mechanisms of the host cell injury have not been elucidated though cell membrane injury by phospholipase A and protease enzymes has been proposed.
|
|
|
Copyright © 2022 histopathology-india.net

