|

Custom Search
|
|
Infectious Disease Online Pathology of African Trypanosomiasis (Sleeping Sickness)
|
|
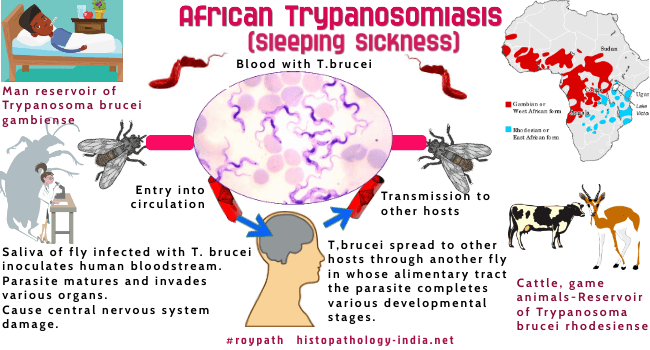
Human African Trypanosomiasis or sleeping sickness, is a disease caused by Trypanosoma brucei gambiense or Trypanosoma brucei rhodesiense. Humans are the main reservoir of both forms. These hemoflagellate protozoa are transmitted by the bite of various species of Glossina, the tsetse fly. The trypanosomes give rise to two distinct clinical entities, Gambian trypanosomiasis (chronic infection) and Rhodesian trypanosomiasis (acute infection). The uneven distribution of African trypanosomiasis is related to the habitats of tsetse flies. African trypanosomiasis is limited to a wide belt of territory in the African continent between the latitudes of 10 degrees north and 25 degrees south. Neither type is present at elevations over 7000 feet above sea level. Related post: American Trypanosomiasis (Chagas' Disease) In Gambian trypanosomiasis, Trypanosoma brucei gambiense is transmitted by tsetse flies of the riverine bush, mainly in focal areas of West and Central Africa. Man is the only important reservoir for Trypanosoma brucei gambiense, which cause a chronic lesion often lasting more than a year. In Rhodesian trypanosomiasis, Trypanosoma brucei rhodesiense is transmitted by tsetse flies of the woodland savanna of East Africa. Antelope, other game animals and domestic cattle are natural reservoirs of Trypanosoma brucei rhodesiense. Incidental infection of man is an occupational hazard of game wardens, fisherman and cattle herders. Trypanosoma brucei rhodesiense causes a disabling, acute, fulminant infection in man, killing the patient in 3 to 6 months.
The clinical manifestations of trypanosomiasis are divided into: Stage 1 - Primary Chancre and systemic infection excluding the brain ; Stage 2 - Invasion of the brain. A firm, tender, reddened nodule may develop in a matter of a few days at the site of the bite. Trypanosomes may be identified in Giemsa-stained smears of fluid aspirated from the nodule. The ulcerated nodule, or "trypanosomal chancre", is accompanied by a regional lymphadenitis that lasts 1 or 2 weeks. The rapidity of the development of the chancre is related to the number of trypanosomes transmitted. The chancre precedes parasitemia. The hemoflagellates apparently reach the bloodstream via lymphatics. This is followed within 1 to 5 weeks by the onset of fever, sweating, general malaise and a generalized lymphadenitis often involving involving primarily the posterior cervical glands. Frequently there are transient skin eruptions characterized by erythema or edema. These symptoms and signs may progress to the phase of central nervous system. Numerous trypanosomes are found in the blood soon after infection, specially after symptoms have developed. Other hematologic findings may include anemia, granulocytopenia and thrombocytopenia. There is an increase in sedimentation rate and a hypergammaglobulinemia specially of the IgM class. Patients have high levels of circulating immune complexes, which are believed to lead to immune complex-mediated vasculitis. Lymph node enlargement, particularly of the posterior cervical lymphnodes (Winterbottom's sign), is a common clinical feature. The lymph nodes contain numerous parasites, and there is a generalized hyperplasia of lymphoid and reticular elements. Fibrosis of the lymph nodes develops later, with reduction in their size. Trypanosomes evade the immunologic response of the host by presenting to the immune system progressively different surface glycoprotein constituents. By the time the host mounts an immune response, the trypanosome has new surface antigens to which the formed antibodies are not specific. This phenomenon of antigenic variation is accomplished by the trypanosome through a mechanism of gene conversion and DNA rearrangement. Trypanosomes also are known to cause immunosuppression by limiting specific antibody response, specially of the IgG type. The host is left with nonspecfic IgM production to combat the infection. This partially explains the rise in IgM levels in this chronic infection. Although there is much overlap between the clinical manifestation of T. brucei gambiense and T. brucei rhodesiense infections , the latter usually follows a much more acute course. Untreated persons with T. brucei rhodesiense infection frequently die within 3 to 6 months after onset of the disease. The systemic stage is often characterized by serous effusions and evidence of pancarditis. The parasites in the Rhodesian variety, after entering the lymph nodes, produce toxic substances that cause hyperplasia of the endothelial lining of the blood sinuses and perivascular infiltration of leukocytes. Only rarely does the victim survive long enough for the trypanosome to invade the central nervous system and produce lesions characteristic of the third stage of T. brucei gambiense infection. The neurologic symptoms and signs, when present are similar to those of gambian trypanosomiasis. Gambian trypanosomiasis is characteristically a chronic disease. In the third stage the patient becomes indifferent, apathetic and drowsy. Focal neurologic signs are uncommon, though athetosis, chorea, and sphincter disturbances may become apparent. The syndrome resulting from invasion of the central nervous system is commonly referred to as " sleeping sickness," but this designation suggests only one of the more advanced neurologic symptoms. In the majority of cases there are no major macroscopic alterations in the brain substance other than edema and occasionally petechiae. Microscopically, the picture is that of a diffuse meningoencephalitis. There is mononuclear infiltration of the superficial leptomeninges , sulci and Virchow-Robin spaces. The cellular infiltrate composed of lymphocytes and plasma cells in various proportions, may also infiltrate the white matter and to a lesser extent the gray matter. The morular cell described by Mott is a plasma cell whose cytoplasm contains numerous Russell bodies, which coalesce and partially or totally hide the nucleus of the cell. Although these cells are not pathognomonic of trypanosomiasis, their presence in large numbers is fairly characteristic of the disease. Diagnosis of the disease: The simplest diagnostic test is the demonstration of the trypanosomes in the circulating blood during febrile episode. Lymph node imprints may be useful for the identification of the parasite. Examination of the cerebrospinal fluid reveals trypanosomes as the disease progresses and may serve as an index of the course of the disease. The greatest elevation of IgM in both the serum and cerebrospinal fluid can be used as a screening diagnostic test. Serodiagnosis is available by indirect immunofluorescence, complement fixation and enzyme-linked immunosorbent assay (ELISA). Treatment: The key drugs used for therapy of African trypanosomiasis are pentamidine, for chemoprophylaxis ; suramin, for the treatment of the early disease in which trypanosomes are found in the blood, lymph, and lymph nodes ; and melarsoprol, for the later disease in which trypanosomes are located in the brain.
|
|
|
Copyright © 2022 histopathology-india.net

