|

Custom Search
|
|
Infectious Disease Online Pathology of Leishmaniasis Dr Sampurna Roy MD 2022
|
 |
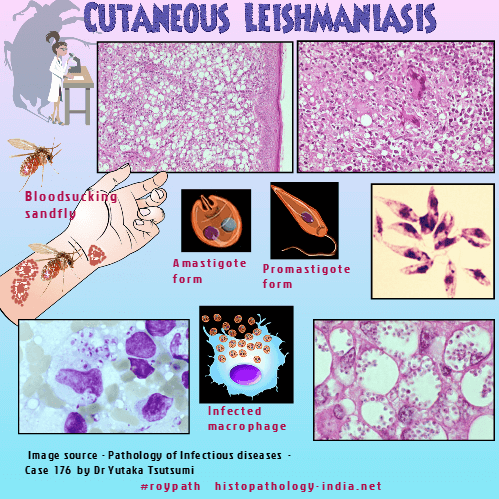
| Leishmaniasis is a
chronic inflammatory disease caused by obligate intracellular
kinetoplastid protozoan parasites, which are transmitted through the
bite of infected sandflies. Life Cycle: Blood-sucking sandflies ingest amastigotes from an infected host. These are transformed in the sandfly gut into promastigotes, which multiply and are injected into the next vertebrate host. There they invade reticuloendothelial cells, transform into amastigote form and multiply, eventually rupturing the cell. They then invade other reticuloendothelial cells thus completing the cycle.
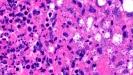
Cutaneous Leishmaniasis: 1. Acute lesions: Present as a papule or nodule. The lesion may ulcerate and heal leaving a scar. Clinical differential diagnosis : Deep fungal infection and atypical mycobacteria. Microscopic feature: - Dense dermal infiltrate of lymphocytes, plasma cells, histiocytes, epithelioid cells and occasionally eosinophils and giant cells. Sometimes neutrophils are present throughout the reticular dermis. - Numerous parasitized macrophages. The organisms are round to oval basophilic structures with eccentrically located kinetoplast. - The parasites lack capsule (Differential diagnosis: Histoplasma Capsulatum) - Organisms located at the periphery of the macrophages-"marquee" sign - Oedema in the upper part of the dermis (+/-). - Epidermis-
Shows hyperkeratosis and acanthosis but sometimes
atrophy. May be ulcerated.
Usually single sometimes multiple, non ulcerated raised plaques. Persists for 1 to 2 years. Microscopic features: Parasitized macrophages are reduced in number Small tuberculoid granulomas composed of epithelioid cells, histiocytes and occasional giant cells. Epidermis shows atrophy Mild to moderate mononuclear infiltrate (lymphocytes & plasma cells) near the granuloma together with fibrosis and telangiectasia. Differential diagnosis: (i) Lupus vulgaris ; (ii) Tuberculoid leprosy - Granulomas are elongated-present along neurovascular plexuses. 3. Recidivous (lupoid) form: Erythemous papules often present at the periphery of a scar of a healed acute lesion. Clinically resemble lupus vulgaris. Microscopic features: Consists of tubercles surrounded by lymphocytes, histiocytes & giant cells. There is no necrosis. Occasional plasma cells. Organisms are fewer in number and found only after careful examination of the section. Differential diagnosis : Lupus Vulgaris and tuberculoid leprosy. 4. Disseminated Anergic form: Primary diffuse cutaneous leishmaniasis. Clinical presentation: Widespread nodules and macules without ulceration. There no involvement of other viscera. Microscopic features: Consists of dense diffuse dermal mixed inflammatory cellular infiltrate together with numerous parasitized macrophages. Differential diagnosis: Lepromatous leprosy- Consists of histiocytes with bluish gray cytoplasm-confirmed by Fite's stain. Mucocutaneous Leishmaniasis Initially lesions resemble cutaneous leishmaniasis. In some cases destructive ulcerative lesions develop at the mucocutaneous junctions of larynx, nasal septum, anus and vulva. Microscopic features: Parasitized macrophages are reduced in number. There may be occasional tuberculoid granulomas. Presence of necrosis with reactive response is a favourable prognostic feature. Visceral Leishmaniasis (Kala-azar): Parasites invade macrophages throughout the reticuloendothelial system and cause severe systemic marked by hepatomegaly, lymphadenopathy, pancytopenia, fever and weight loss. Often there is hyperpigmentation of the skin in the extremities. 'Kala-azar' is a Hindi word meaning black fever. Post- kala-azar dermal leishmaniasis develops in about 5% of cases of visceral leishmaniasis. It is mainly seen in Sudan and India. Post- kala-azar dermal leishmaniasis follows visceral leishmaniasis after an interval of 0-6months in Sudan and 2-3 years in India. The patient presents with areas of erythema (face), macules (trunk) and nodules (face and limbs). The rash starts around the mouth and then spreads to the rest of the body. Clinically the differential diagnosis is leprosy (no loss of sensation in PKDL). Cases have also been reported in HIV (+) patients. Microscopic features: A dense infiltrate of inflammatory cells composed of lymphocytes,
plasma cells, macrophages, epithelioid cells.
In nodular
lesions the inflammatory infiltrate may be The parasites (Leishman Donovan bodies) can be easily detected by Giemsa stain.
|
|
|
 |
Copyright © 2002-2022 histopathology-india.net