|

Custom Search
|
|
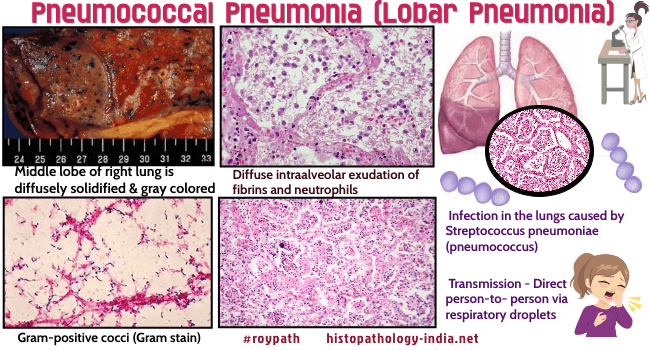
Infectious Disease Online Pathology of Pneumococcal Pneumonia (Lobar Pneumonia)
|
|
Pneumococcal
pneumonia is an infection in the lungs caused by bacteria called
Streptococcus pneumoniae
(also called pneumococcus ). Streptococcus pneumoniae is a Gram-positive coccus that may be found in pairs or in short chains. Lobar Pneumonia involves large portion of a lobe or an entire lobe of the lung . Pneumococcal pneumonia is of diminishing significance because of prompt response to treatment, it is still a significant illness in industrialized nations. In the non-industrialized world it is still a major cause of mortality. It is commonly a disease of healthy young to middle-aged adults, is rare in infants, and the elderly, and is considerably more common in men than in women. Alcoholics appear to be particularly vulnerable. It can infect the upper respiratory tracts of adults and children and can spread to the blood, lungs, middle ear, or nervous system. Pneumococcal pneumonia is commonly seen in young adults after exposure to cold or after previous respiratory infection. It typically follows a viral infection, often influenza. The onset of the disease is sudden with fever and chills and ends in crisis after 9-10 days. Chest pain due to pleural involvement is common, as is hemoptysis, which is characteristically “rusty”, since it is derived from altered blood in alveolar spaces. Radiologic examination shows alveolar filling in large areas of lung, producing a solid appearance that extend to entire lobes or segments. Although the symptoms of pneumonia respond rapidly to antibiotic therapy, radiologically the lesion still takes several days to resolve. Before antibiotic therapy the clinical course was characterized by severe fever, dyspnea, debility, and even loss of consciousness. The satisfactory resolution of a crisis is the result of a good immune response to the infection. However, often the outcome is not favorable and the patient dies. Sequence of stages is described in 4 phases: All 4 phases may be seen in different parts of the same lung. 1. Congestion (1-2 days) 2. Red hepatization (2nd-4th day) 3. Gray hepatization (4th-6th day) 4. Resolution (8th-9th day) In the earliest stage of pneumococcal pneumonia, protein-rich edema fluid containing numerous organisms (Streptococcus pneumoniae) fills the alveoli. Marked congestion of the capillaries is typical. Shortly after this congestion occurs there is a massive outpouring of polymorphonuclear leukocytes accompanied by intra-alveolar hemorrhage. Many of the red blood cells undergo lysis. These cells, together with polymprphonuclear leukocytes, produce the rusty sputum. Because the firm consistency of the affected lung is reminiscent of the liver, this stage has been named "red hepatization". The next phase, occurring after 2 or more days, depending on the success of treatment, involves the lysis of polymorphonuclear leukocytes and the appearance of macrophages, which phagocytose the fragmented polymorphonuclear leukocytes and other inflammatory debris. The lung is now no longer congested but still remains firm in this stage of "gray hepatization". The alveolar exudates is then removed and the lung gradually returns to normal. A painful pleuritis is common because the pneumonia often extends to the pleura. There is usually a small pleural effusion, which resolves. However, this may occasionally be large and purulent (pyothorax) and may heal with extensive fibrosis. Rarely, the purulent exudates persists and leads to a loculated collection of pus with fibrous walls (empyema). Bacteremia is usually present in the early stage and may result in endocarditis or meningitis. Rarely, the alveolar lesion proceeds to fibrosis, in which case the intra-alveolar exudates becomes organized as fibroblasts leads to a shrunken and firm lobe, a rare complication known as “carnification”. Another uncommon outcome is a lung abscess. Little is known about the precise pathogenesis of pneumococcal pneumonia. The frequency of a previous respiratory tract infection suggests that impairment of airway clearance mechanisms may be important. It has been suggested that the organisms can multiply rapidly in the increased airway mucus and may then be aspired into the periphery. The remarkably severe acute inflammation with spreading edema has led to speculation that immunologic mechanisms may be involved Cause of death: Toxemia with peripheral circulatory failure. Complications of pneumonia: 1. Delayed resolution. 2. Abscess formation . 3. Empyema 4. Organization of exudates with fibrosis. 5. Bacteremia and septicemia with infection to other organs. Example- endocarditis, pericarditis, meningitis, arthritis etc.
Pathogenesis: Sudden onset & pathological changes suggest the role of hypersensitivity in the pathogenesis. Previous infection sensitizes the lungs, so that subsequent infection may result in pneumonia. Pneumococci reach alveoli via bronchial tree. They pass in the inflammatory fluid from one alveolus to another through the alveolar pores of Cohn. Thus infection spreads throughout the entire lobe. Edema producing substances of capsular polysaccharide cause marked inflammatory edema with acute inflammatory exudates filling up alveoli. The lung is converted into a solid & airless organ. The process is known consolidation or hepatization (liver-like in consistency). Pathology: 1.Congestion: Gross: (i) Lungs are dark-red color and pits on pressure (due to edema). (ii) Cut surface: bloodstained frothy fluid comes out. Microscopic features: (i) Alveolar capillaries are dilated. (ii) Alveoli contain edema fluid and pneumococci. (iii) Air is still present in the alveoli. 2. Red hepatization: Gross: (i) Affected part of the lung is consolidated, reddish-brown and sinks in water. It is friable. (ii) Outer surface is covered with fibrinious exudates. (iii)Cut surface is rough, dry and granular. Microscopic feature: i) Alveoli are airless andfilled up with inflammatory exudates consisting of red blood cells (RBCs), neutrophils and fibrin strands. ii) Alveolar wall is thick (due to edema) with congested blood vessels (In low power -mosaic appearance) 3. Grey hepatization: Gross: (i) Consolidated part is gray colour and more friable. (ii) In outer surface pleural exudates is thicker. (iii) Cut surface is moist and brownish-gray colour (bronchial lymphnodes may be enlarged). Microscopic features: (i) Alveolar exudates have lost their freshness (due to action of proteolytic enzymes). RBCs are ghosts, nuclei of polymorphs are broken and indistinct and fibrin threads contract to form a clear zone adjacent to alveolar wall. (ii) Alveolar wall is thin (due to lack of edema) and congested blood vessels disappear. 4. Resolution: Gross: Lung is soft and translucent (jelly like). Microscopic features: (i) Macrophages invade exudates. (ii) Alveolar exudates is liquefied by proteolytic enzyme & removed. Thus the consolidated lung is restored to normal.
|
|
|

