|

Custom Search
|
|
Infectious Disease Online Pathology of Sporotrichosis |
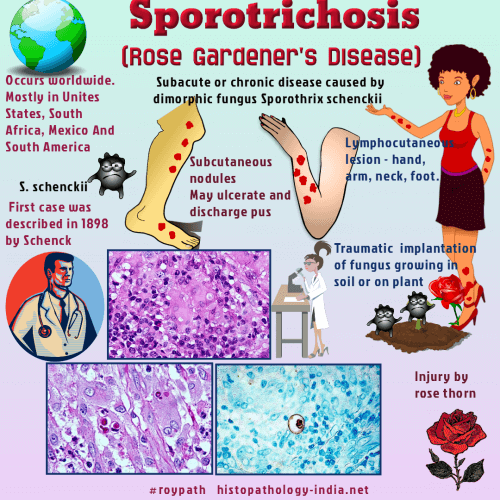
Syn: Rose Gardener's Disease ; Rose Thorn Disease Sporotrichosis is a subacute or chronic disease caused by the dimorphic fungus Sporothrix schenckii. The organism derives its name from RB Schenck, who first reported the infection in 1898. Geographic distribution: The disease occurs worldwide, but most reported cases have originated from the United States, South Africa, Mexico, and South America. Mode of infection: Infection usually results from the traumatic implantation of the fungus, growing in soil or on plant materials, into the skin and subcutaneous tissue. In rare instances, a primary cutaneous infection may disseminate to the bones, joints, lungs, and other organs. Even more rarely, inhalation of the fungus results in primary pulmonary infection, which may disseminate. Sporotrichosis is not contagious, but infection can result from contamination of skin wounds with exudates from humans or animals with sporotrichosis. There is no evidence that underlying disease or immunosuppression predispose to a person to infection. Clinical presentation: The most common form of sporotrichosis is lymphocutaneous. Clinically, this form is manifested as a chain of subcutaneous nodules along the course of lymphatics draining a primary skin lesion that may be nodular and ulcerated. Lymphocutaneous lesions develop within 7 to 90 days or longer after penetrating injury to an exposed part of the body, such as the hand, arm, neck, or foot. Eventually, the subcutaneous nodules soften, ulcerate, and discharge pus. Solitary, ulcerated, and verrucous lesions of the skin without lymphatic involvement also occur. They are sometimes mistaken for a neoplasm and excised surgically. Sporotrichosis schenckii usually elicits a mixed suppurative and granulomatous inflammatory reaction accompanied by microabscess formation and fibrosis. This type of inflammation is typical of all forms of the disease, but it is not specific. In tissue sections, Sporotrichosis schenckii appears as spherical, oval, or elongated (cigar-shaped) yeast-like cells, 2 to 6 micrometer or more in diameter. The fungal cells often bear elongated buds with narrow-based attachments to the parent cells. Multiple budding is seen rarely. Although considered by some to be the classic tissue form of the fungus, cigar-shaped organisms are not commonly found. When present, they are most often observed in disseminated lesions. Hyphae are rarely found in tissue. The presence of asteroid bodies (fungal cells surrounded by Splendor-Hoeppli material) within microabscesses is helpful in making a presumptive histologic diagnosis of sporotrichosis. However, the asteroid body is not pathognomonic for the disease. Splendore-Hoeppli material may surround parasitic ova, actinomycotic granules, eumycotic granules, foreign objects such as silk sutures, and other species of fungi, especially Coccidioides immitis , Aspergillus and Candida . In many cases of sporotrichosis, asteroid bodies cannot be detected.
Diagnosis: Generally, few Sporotrichosis schenckii cells are found in cutaneous lesions, and special stains for fungi, complemented by immuno-flourescence staining, are needed to identify the fungus in fixed tissues. When immunoflourescence tests are not available, microbiologic culture or mouse inoculation is essential for an accurate diagnosis. Treatment: The treatment of choice for sporotrichosis is potassium iodide, especially for lymphocutaneous infection. Amphotericin B and other antifungals may also be useful in systemic infection. If untreated, the infection may persist for years.
|
|
|
Copyright © 2022 histopathology-india.net

