|

Custom Search
|
|
Dermpath-India Pathology of Infantile Hemangioma
|
| Syn: Benign Infantile Hemangioendothelioma; Cellular Hemangioma of Infancy; Juvenile Hemangioma;
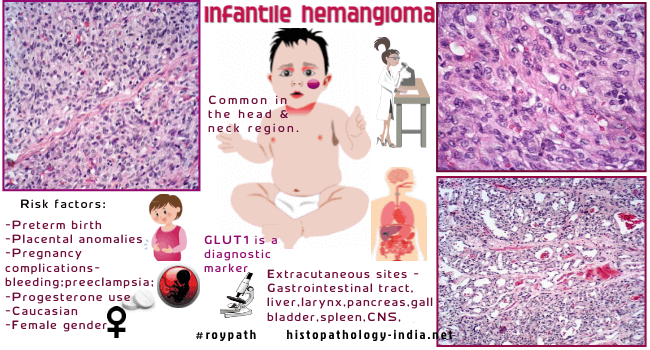
Strawberry nevus. Infantile hemangiomas, the most common tumours of infancy, are vascular tumours characterized by rapid proliferation of endothelial cells during the first few months of postnatal life followed by slow spontaneous involution. Pathogenesis of hemangioma is not understood. Growth factors and hormonal and mechanical influences have been postulated to affect the abnormal proliferation of endothelial cells in hemangioma. The primary, causative defect in hemangiogenesis is not known and no genetic alteration has been implicated. Total regression of the lesion occurs in most cases and usually there is no need for surgical intervention. Periorbital lesions require active therapy because of associated visual complications. Segmental hemangioma (affecting particular area of skin) may be associated with underlying anomalies of heart, blood vessels or nervous system. Age and sex: This immature form of capillary hemangioma occurs during infancy. It occurs in almost 3% to 10% of newborn population. It is common in premature infants. Females are affected slightly more often than males. Clinical presentation: The lesions usually appear in the first few weeks of life. Infantile hemangioma clinically demonstrates an early period of growth and is usually followed by a stationary period and then, over several years, a phase of slow regression. In the early stage these are flat, red or purple macules which gradually acquire an elevated protruding appearance. The lesion usually reaches its maximum size by 3-6 months. Site: Head and neck area, trunk, extremities. Extracutaneous sites include gastrointestinal tract, liver, larynx, pancreas, gall bladder, spleen, central nervous system, adrenal gland, lymph node, urinary bladder and lung. Microscopic features: Image Links: Images of Infantile hemangioma The early lesions display solid, cellular lobules consisting of plump endothelial cells lining tiny rounded vascular spaces with inconspicuous lumina. [Practical clue- At this stage a reticulin stain is useful in demonstrating the connective tissue fibres encircling the tiny vessels ]. Moderate numbers of mitotic figures are present. There may be numerous mast cells in the stroma. Vascular proliferation may involve subcutaneous tissue and may partly or completely replace the fat lobules. (Differential diagnosis - Angiolipoma). Vascular proliferation is also noted around sweat glands. Perineurial invasion in infantile hemangiomas is a relatively common finding and should not be regarded as evidence of malignancy. Maturation usually commences at the periphery of the lobules and is accompanied by an enlargement of vascular spaces and flattening of the endothelium. The regressed lesions display: progressive fibrosis ; absence of vascular elements; fat replacement of vascular tissue in the subcutis. High endothelial immunoreactivity for the erythrocyte-type glucose transporter protein GLUT1 is a specific feature of juvenile/ infantile hemangiomas during all phases of these lesions. This is a highly selective and diagnostically useful marker for infantile hemangiomas. Cytogenetics:
A locus for an autosomal dominant predisposition has
been identified on chromosome 5q. Infantile hemangiopericytoma: The cells in hemangiopericytoma lie outside the vascular sheath ; in capillary hemangioma these cells are contained within the vascular sheath. A reticulin stain and immunohistochemistry for smooth muscle actin may be useful in establishing the diagnosis. Kaposiform Haemangioendothelioma; Tufted Hemangioma; Pyogenic granuloma. (Negative for GLUT-1) Congenital Hemangiomas : Occasional "hemangiomas" differ from the infantile form in presenting fully formed at birth, then following a static or rapidly involuting course. RICH (rapidly involuting congenital hemangioma) and NICH (noninvoluting congenital hemangioma). 1. Rapidly involuting congenital haemangioma. Clin Exp Dermatol. 2009 Dec;34 (8):937-8. 2. Rapidly involuting congenital haemangioma associated with transient thrombocytopenia and coagulopathy: and coagulopathy: a case series.Br J Dermatol. 2008 Jun;158(6):1363-70. Epub 2008 Apr 10. Congenital nonprogressive hemangiomas - Features: Lobules of capillaries set within densely fibrotic stroma containing hemosiderin deposits; focal lobular thrombosis and sclerosis; frequent association with multiple thin-walled vessels; absence of "intermingling" of the neovasculature with normal tissue elements; and lack of immunoreactivity for GLUT1 and LeY. Dermatopathology Quiz Case - 103
|
| Diffuse Neonatal
Hemangiomatosis:
Multiple cutaneous hemangiomas may occur with or without disseminated visceral hemangioma. Other developmental anomalies may be present with this condition. Patients with visceral involvement has a poor prognosis. Death usually occurs within a few months of birth. Cause of death: High output congestive cardiac failure (particularly in liver) ; Central nervous system complications; bleeding associated with Kasabach- Merritt syndrome. Benign neonatal hemangiomatosis: Purely cutaneous form of hemangiomatosis with good prognosis. PHACES - Posterior fossa malformations (Arnold-Chiary and Dandy Walker malformations) Hemangiomas- (large plaque like facial lesion) Arterial anomalies (carotid or vertebral), Cardiac anomalies (coarction of aorta), Eye abnormalities, Sternal clefts and or supraumblical raphe.
Further reading: Diffuse neonatal hemangiomatosis: a new constellation of findings. Benign cutaneous vascular tumors of infancy: when to worry, what to do. Miliary neonatal hemangiomatosis with fulminant heart failure and cardiac septal hypertrophy in two infants. Benign neonatal hemangiomatosis: review and description of a patient with unusually persistent lesions. Benign neonatal hemangiomatosis with aggressive growth of cutaneous lesions. Haemangiomas and diffuse neonatal haemangiomatosis.
|
|
|


