|

Custom Search
|
|
Infectious Disease Online Pathology of Infective Endocarditis
|
|
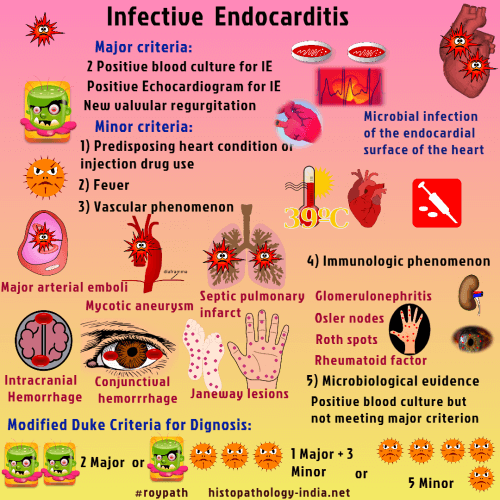
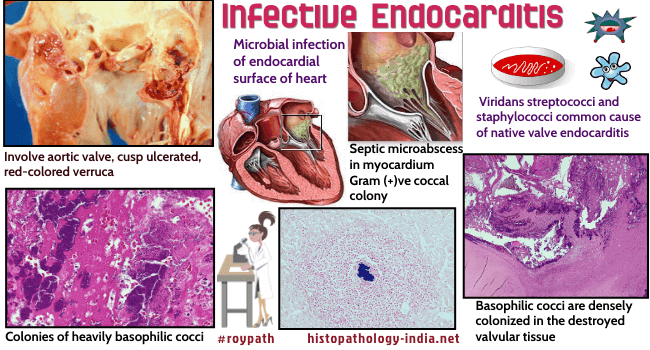
Infective
endocarditis, a microbial
infection of the endocardial surface of the heart. It has been classified as "acute" or "subacute - chronic" on the basis of severity of the clinical presentation and the progression of the untreated disease. The characteristic lesion, a vegetation, is composed of a collection of platelets, fibrin, microorganisms, and inflammatory cells. It most commonly involves heart valves but may also occur at the site of a septal defect, on the chordae tendineae, or on the mural endocardium. Men are more often affected than women. Clinical features: Fever ; Cardiac manifestations ; Evidence of embolisms. Fever is the most common symptom and sign; however, it may be absent or minimal in patients with congestive heart failure, severe debility, chronic renal or liver failure. Other common symptoms of subacute infective endocarditis include anorexia, weight loss, malaise, and night sweats. Most patients with infective endocarditis have a heart murmur (most commonly preexisting), and patients may have petechiae on the skin, conjunctivae, or oral mucosa, as well as splenomegaly and other peripheral manifestations. Unexplained fever in a patient with a prosthetic valve should prompt careful evaluation for prosthetic-valve endocarditis. In earlier literature the term "subacute" was used to refer infections that were from 6 weeks to 3 months or more in duration. The term "acute" was applied to patients who died in less than 6 weeks. Current effective treatment has changed the course of the two varieties of endocarditis , so there is now an overlapping in their clinical, bacteriologic and pathologic features. Causative organism: Viridans streptococci and staphylococci are the most common causes of native valve endocarditis. Coagulase negative staphylococci and Staphylococcus aureus are more commonly seen in cases of prosthetic valve endocarditis. Infection by other forms of streptococci (including enterococci), gram-negative organisms, and various unusual organisms have increased in incidence. Fungal endocarditis from Candida albicans, Histoplasma capsulatum, Coccidioides immitis, Aspergillus, Cryptococcus neoformans, Blastomyces dermatitidis, and Mucor has been reported. Other commonly implicated organisms include the HACEK group, (Haemophilus aphrophilus, Haemophilus paraphrophilus, Haemophilus influenzae, Haemophilus parainfluenzae, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella species), Coxiella burnetii , Bartonella , Brucella and Legionella . Predisposing factors: The development of Infective Endocarditis requires: (i) The presence of infective organisms in the bloodsream ; (ii) Preparation of the valve surface to permit adherance and subsequent proliferarion of circulating organism. Conditions associated with an increased incidence of infective endocarditis include poor dental hygiene, long-term hemodialysis, and diabetes mellitus. The highly pathogenic organisms that produce endocarditis commonly arise from infections elsewhere in the body (such as pneumonia, skin infections and renal infections) or may be introduced intravenously by narcotic addicts. Human immunodeficiency virus (HIV) infection and infective endocarditis are serious complications of injection drug use. Staphylococcus aureus is the most frequent pathogen in these patients, and mortality is higher among those with advanced HIV disease. The presence of underlying heart disease predisposes to infective endocarditis. In a number of cases of rheumatic fever organisms are implanted on the valves that are thickened and fibrotic. Mitral-valve prolapse is now the most common cardiovascular diagnosis predisposing patients to infective endocarditis. Atherosclerotic aortic valvular disease may also predispose to infective endocarditis. Congenital lesions predisposing to the infection include bicuspid aortic valves , interventricular septal defects, subaortic stenosis and pulmonary stenosis (including tetralogy of Fallot), coarction of the aorta, and patent ductus arteriosus. Prosthetic-valve endocarditis accounts for a number of cases of infective endocarditis. Mechanical heart valves are probably at higher risk for infection than are bioprostheses during the first three months after surgery. Cases with onset within two months after surgery are called early prosthetic-valve endocarditis and are usually acquired in the hospital. Cases that occur more than 12 months after surgery are called late prosthetic-valve endocarditis and are largely community-acquired. All cases of endocarditis seen at hospitals are nosocomial. Infected intravascular devices give rise to a number of these cases. Other sources of nosocomial infective endocarditis include genitourinary or gastrointestinal tract procedures or surgical-wound infection.
Pathological Features: The characteristic pathologic feature of infective endocarditis is the presence of vegetations on the valve cusps or leaflets. The valve most frequently affected is the mitral . The aortic valve is the next most commonly involved.Rarely, in narcotic addicts infective endocarditis involves the tricuspid valve. The vegetations vary in size from a few millimeters to a centimeter or more and are gray, reddish, or brown fairly firm but friable single or multiple and flat, filiform, fungating or polypoid. Because the vegetations are friable they give rise to emboli (Differential diagnosis- This is absent in rheumatic lesions).) The vegetations tend to localize on the atrial surface of the atrioventricular valves and on the ventricular surfaces of the semilunar valves. They arise from the contact areas of the cusps or leaflets but tend to spread along the valve surfaces onto the adjacent mural endocardium. The chordae tendineae may be involved. Ulceration and perforation of the valve leaflets or cusps may develop. Microscopic features: Microscopically, the vegetations consist of fibrin, platelets, leukocytes, and the infecting organism, and in the underlying valve a nonspecific inflammatory reaction with varying degrees of necrosis is present. In the acute, fulminant cases, neutrophils are prominent, and there may be extensive necrosis with abscess formation. The abscess may extend to the valve rings. In the prolonged cases, varying degrees of granulation tissue and fibroblastic proliferation with mononuclear inflammatory cells are seen. Sometimes foreign-body giant cells are noted in the necrotic area. Bacterial masses may be present in the periphery of the fibrin, in a position to seed the bloodstream with organism. Healing of the vegetation may take place, particularly after antibiotic therapy. There is invasion of the fibrinous layer by granulation tissue, resulting in fibrosis. Hyalinization, calcification and endothelialization of the vegetation subsequently occur. If calcification is extensive a severely deformed nodular valve may occur. In fungal endocarditis microscopically many organisms are usually present in the vegetations. The inflammation of the underlying endocardium is consistent with the nature of the infecting organisms and includes granulomatous or acute and chronic nonspecific inflammation with or without suppuration.
|
|
|