|

Custom Search
|
|
Dermpath-India Pathology of Microcystic Adnexal Carcinoma Dr Sampurna Roy MD 2022
|
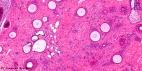
Microcystic Adnexal Carcinoma a slow growing locally aggressive adnexal tumour was first reported by Goldstein et al, in 1982. This tumour shows both eccrine and pilar differentiation. However, it has been recently regarded as an apocrine tumour. Clinical presentation: The tumour usually presents as skin coloured indurated plaque or nodule. Site: The lesion usually occurs on the upper lip or elsewhere on the face. It is also noted in the axilla, extremities, genital skin, trunk and scalp. Locally Aggressive Adnexal Tumour- Microcystic Adnexal Carcinoma [Pathology Infographic
Differential
Diagnosis: Desmoplastic trichoepithelioma and syringoma do not show evidence of aggressive growth pattern and perineural spread. It is not possible to give a definitive diagnosis in shave or superficial punch biopsies. In morpheic basal cell carcinoma there is no lumen formation or zonation of the tumour. Mohs micrograph surgery is the current treatment of choice. Local recurrence occurs in 50% cases. This is less likely if excision margins are free of tumour in the initial biopsy. |
|
|