|

Custom Search
|
|
Infectious Disease Online Pathology of Yellow Fever
|
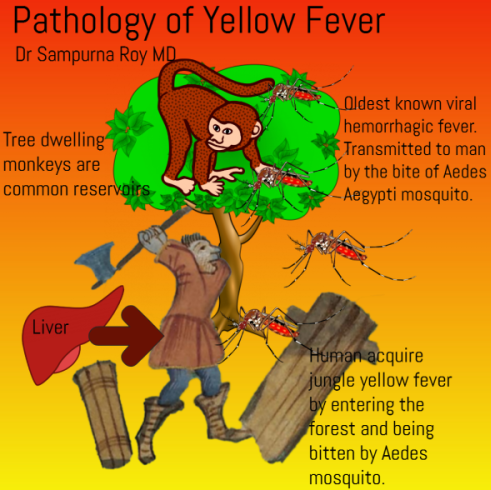
Yellow fever (YF) is an infectious, non-contagious disease caused by a RNA virus of the family Flaviviridae (that cause dengue and other hemorrhagic fevers), which is transmitted to man by the bite of hematophagous mosquitoes. First described in the Caribbean, yellow fever is the oldest known viral hemorrhagic fever. It is a re-emerging infectious disease that currently is at risk of urbanization due to the advance of the Aedes aegypti vector. Geographic distribution: The disease affects about 200,000 individuals annually, mainly in tropical Africa and South America, including both jungle and urban settings. It is a significant hazard to unvaccinated travelers to these endemic areas. Recent increases in the density and distribution of the urban mosquito vector, Aedes aegypti, as well as the rise in air travel increase the risk of introduction and spread of yellow fever to North and Central America, the Caribbean, the Middle East, Asia, Australia, and Oceania. Mode of Infection:
The usual reservoir is tree dwelling monkeys, virus being passed among them in the forest canopy by mosquitoes. These monkeys are a good reservoir because the virus neither kills them nor makes them ill . Humans acquire jungle yellow fever by entering the forest and being bitten and inoculated by Aedes mosquitoes. Felling trees increases the risk because mosquitoes are brought down with the tree. On returning to the village or city, the victim becomes the reservoir for epidemic yellow fever in the urban setting , where Aedes aegypti is the vector. Hence, virus transmission occurs between humans, mosquitoes, and monkeys. The mosquito, the true reservoir of Yellow fever, is infected throughout its life, and can transmit the virus transovarially through infected eggs. Man and monkeys, on the other hand, play the role of temporary amplifiers of the virus available for mosquito infection. Clinical presentation: This is an acute illness manifested by abrupt onset of chills and fever, conjunctival injection, leukopenia, a brief period of remission, and then reappearance of fever and jaundice, punctate hemorrhages of the soft palate, epistaxis, and gingival and gastrointestinal bleeding (black vomit). Approximately 50% of the patients develop relative bradycardia in relation to the degree of fever. Death occurs in the second week after onset,and is preceded by coma. Pathogical features: The yellow fever virus (YFV) is viscerotropic causing the most damage in the heart, kidneys, central nervous system, gastrointestinal tract and liver. The gross features in fatal cases are not specific. Heart: The heart when involved is flabby and pale with scattered pericardial and petechial hemorrhages. Microscopically there is degeneration of myocardial fibers and accumulation of fat. Kidneys: May show edema ; Microscopically the features are those seen in cases of tubular necrosis. Hemoglobin casts may be seen. The most characterisitic pathologic changes are seen in the liver. The appearance of the lesions is typical between the seventh and ninth day of illness.
Liver: The liver is grossly normal in size, pale and yellow because of fatty metamorphosis. The histopathological pattern is characterized by mid-zonal steatosis, lytic necrosis and hepatocyte apoptosis associated with a moderate mononuclear inflammatory infiltrate. The inflammatory component mainly consisted of CD4+ T lymphocytes, followed by CD8+ T lymphocytes, which showed a preferential portal and midzone distribution. The midzonal necrosis in severe cases may extend to become panlobular. [ A new hypothesis has been proposed that the mid-zonal necrosis is consequence of action of combined factors mainly the direct cytopathic effect of YFV associated with a potent immune response in which CD4+ and CD8+ lymphocytes and the cytokines, especially TGF-beta, but also TNF-alpha and IFN-gamma play an important role.] Intracellular condensations of cytoplasm that appear as round to oval, well-demarcated, eosinophilic inclusions are termed Councilman bodies. These are found in the cytoplasm of Kupffer cells. These inclusions are not composed of virus particles and are nonspecific for the disease. They are periodic acid Schiff (PAS) positive. Rarely, eosinophilic intranuclear inclusions (Torres bodies) are present. Fatty change may be prominent. The surviving liver shows ballooned hepatocytes and regenerative hyperplasia ; multinucleate hepatocytes are common ; Cholestasis is unusual. Biopsies taken from survivors upto 2 months after the acute illness show a non-specific intra-acinar hepatitis. A distinctive feature of the lesion is the fact that despite massive necrosis, the reticulin framework of the hepatic lobule is preserved. This characteristics pattern of liver injury in yellow fever is also observed in conditions of low-flow hypoxia and other infections such as viral hepatitis, dengue, Weil's disease and Rift Valley fever. Brain: Edema and petechial hemorrhage. Spleen and Lymph nodes: Follicular hyperplasia. Skin: Gingiva and Gastrointestinal Tract : Hemorrhage. Diagnosis: The diagnosis is usually confirmed by the serological demonstration of specific IgM by an ELISA method, or by virus isolation from blood.
|
|
|
Copyright © 2022 histopathology-india.net