|

Custom Search
|
|
Infectious Disease Online Pathology of Loiasis
|
|
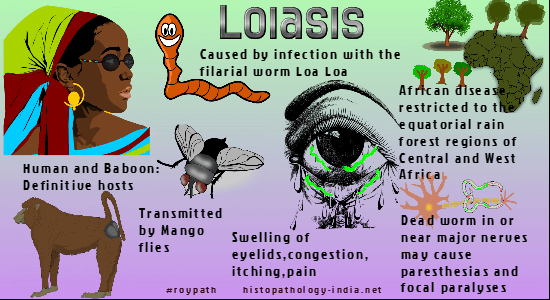
Loiasis is an infectious disease caused by the filarial nematode, Loa loa, the African "eyeworm" or "loa" worm. It was discovered for the first time in the eye of a slave from the Caribbean in 1770. It prevails in the rain forests of central and West Africa. Loiasis is now frequently reported in America, Europe, Australia and Asia. These imported cases cause several problems to the clinician in areas of the world where L. loa is not endemic. Humans and baboons are definitive hosts and infection is transmitted by mango flies (Chrysops species). The adult Loa loa migrates in the skin and occasionally crosses the eye beneath the conjunctiva, making the patient acutely aware of his infection. Gravid worms discharge microfilariae that circulate in the blood stream during the day but reside in capillaries of the skin, lungs, and other organs at night.
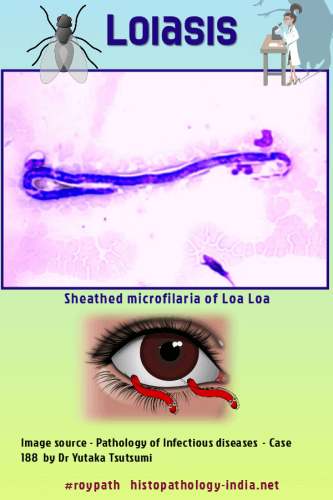
Most infections are asymptomatic but persist for years. Some patients have pruritic, red, subcutaneous, “Calabar” swellings, which may be a reaction to migrating adult worms or to microfilaria in capillaries of the dermis. Ocular symptoms include swelling of lids, congestion, itching, and pain. Female worms, and rarely male worms, may be extracted during their migration beneath the conjunctiva. Systemic reactions include fever, pain, itching, urticaria, and eosinophilia. Dead worms in or near major nerves may cause paresthesias and focal paralyses. Some patients have a regional lymphadenopathy, characterized by follicular atrophy, histiocytic hyperplasia, and eosinophilia. Treatment with microfilariacides may cause massive death of microfilariae and provoke fever, meningoencephalitis, nephritis, coma and death. Migrating worms cause no inflammation, but static worms are surrounded by plasma cells, lymphocytes, eosinophils, neutrophils, fibrin, and a foreign body giant cell reaction. At autopsy patients with acute generalized loiasis have obstructive fibrin thrombi, which contain degenerating, microfilaria, in small vessels of most organs. When the brain is involved, obstruction of vessels by filarial thrombi kills the patient through sudden and diffuse cerebral ischemia. Diagnosis is made by identifying microfilariae in blood films taken during the day, by removal of adult worms from the conjunctiva or by identifying microfilariae or adult worms in biopsy specimens. Visit: Filariasis ; Onchocerciasis ; Dirofilariasis
|
|
|