|

Custom Search
|
|
Infectious Disease Online Pathology of Bartonellosis or Carrion's Disease Acute phase - Oroya Fever
|
Bartonellosis is a group of clinical conditions affecting human beings and a variety of animals.
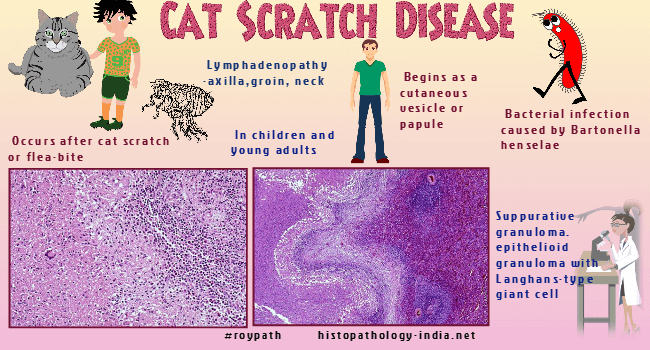
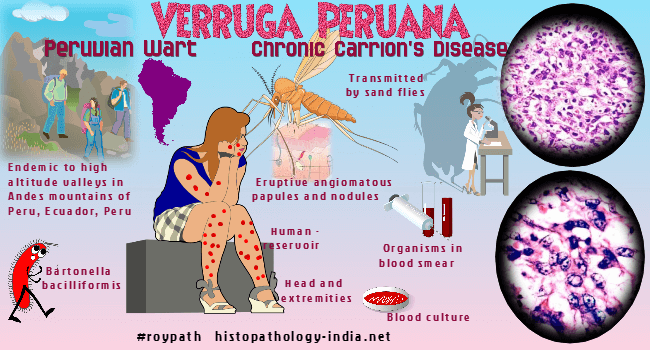
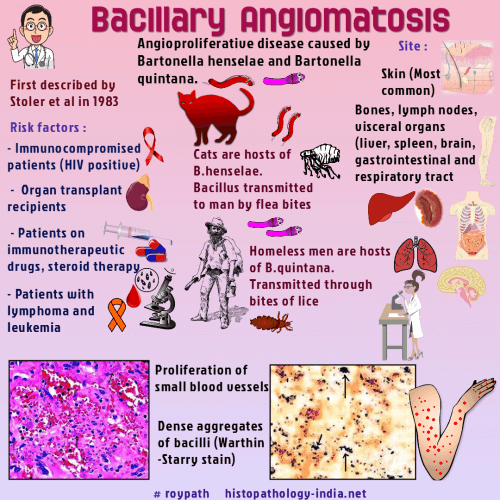
Many Bartonella infections are zoonotic, with some of the most commonly reported zoonotic manifestations of infection including cat-scratch disease, bacillary angiomatosis, endocarditis, and neuroretinitis.Five species of Bartonella have been found to infect humans, henselae, quintana, elizabethae, bacilliformis, and vinsonii.The most common of these in North America are Bartonella quintana and Bartonella henselae, the agents of trench fever, bacillary angiomatosis and parenchymal peliosis, and in the case of Bartonella henselae cat-scratch disease.Bartonella bacilliformis is endemic in Peru and Ecuador, where it causes oroya fever or Carrion's disease.Bartonellosis is an infection by Bartonella bacilliformis , a small pleomorphic, multiflagellated, gram-negative coccobacillus, which is the only member of the genus Bartonella but is closely related to certain animal pathogens. The organisms parasitize erythrocytes in vivo and can be cultured in semisolid media or in embryonated eggs. In smears of blood and in tissue sections stained with Giemsa or Wright stain, the bacteria are reddish-violet. The organisms are small coccobacilli, occasionally curved, and may aggregate in chains of three or in "V" or "Y" forms. The term bartonellosis encompasses two syndromes, both caused by Bartonella bacilliformis - 1) Oroya fever, the acute anemic phase; and 2) Verruga peruana, the chronic dermal phase.
These present as a biphasic pattern, with acute anemic phase first, followed some months later by the chronic dermal phase. Either phase may occur by itself. Visit: Verruga peruana ; cat-scratch disease ; bacillary angiomatosis. Bartonellosis occurs only in Peru, Ecuador, and Colombia. The foci of endemic transmission are river valleys in the Andes at an elevation between 700 and 2,500 meters. The disease is transmitted by the sandflies Phlebotomus verrucarum and Phlebotomus noguchi. The vectors are sensitive to drying and cold, hence the absence of bartonellosis in coastal regions and at higher elevations. Humans provide the only reservoir and acquire bartonellosis at sunrise and sunset, when sandflies are most active. In endemic areas 10% to 15% of the population have latent infections. Newcomers are susceptible, where as the indigenous population is resistant, a difference explained by subclinical infection and immunity in the indigenous people. The incubation period of the acute anemic stage is 3 weeks. The onset is abrupt with fever, skeletal pains, and a severe hemolytic anemia that is often macrocytic. Lymphadenopathy and hepatosplenomegaly are usually present. Reticulocytosis, jaundice, and other changes of hemolytic anemia also occur. The anemia can be profound, and the blood erythrocyte count may fall in a few days from normal to less than 500,000 / micro L. Secondary septicemia caused by salmonellae is frequent and contributes to the high mortality of acute bartonellosis. About 40% of patients with untreated bartonellosis die in the anemic phase. The dermal eruptive phase of bartonellosis sometimes coexists with the anemic phase, but they are usually separated by an asymptomatic interval of 3 to 6 months. Occasionally the eruptive form develops independently without prior evidence of bartonellosis. The eruption is usually military (forma miliar), and many small hemangioma like lesions of the dermis balloon outward and cause a studded appearance. Nodular lesions (forma nodular) are larger but fewer and may be more prominent on the extensor surfaces of the arms and legs. At times, a few large, deep-seated lesions, which tend to ulcerate, develop near joints and limit motion. The eruptive phase is often prolonged, but eventually heals spontaneously. The mortality in eruptive phase is less than 5%. Grossly, the acute phase causes changes characteristic of acute hemolytic anemia, with prominent pallor and jaundice. The bone marrow is hyperplastic. Lymphadenopathy, hepatomegaly, and splenomegaly are present, caused by the engorgement of the reticuloendothelial cells with bacteria, erythrocytes, and hemosiderin.
Serologic tests are not useful. Successful treatment of acute hemolytic bartonellosis has been reported with chloramphenicol, tetracycline, streptomycin, and penicillin but bacteremia is not always eliminated by antimicrobial therapy. Antibiotic therapy of the dermal eruptions has been less successful.
|
|
|