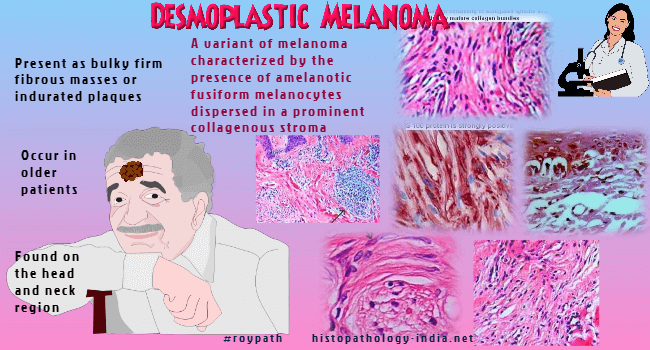
| Desmoplastic melanoma
(DM) is a variant of melanoma characterized by the presence of amelanotic
fusiform melanocytes dispersed in a prominent collagenous stroma.
Desmoplastic neurotropic melanoma (DNM) is
a neurotropic variant of desmoplastic melanoma.
DM and DNM occurred most often in
lentiginous-type melanomas. Lentigo maligna melanoma is associated with
DM and DNM
Clinical presentation:
The clinical presentation of DM and DNM
differs from that of other melanomas. These lesions usually occur in
older patients (median age of 61 years, compared with a median age of 46
years for other melanomas.)
Clinically, the lesions are usually found on the head and neck region and
present as bulky firm fibrous masses of tumour or indurated plaques.
These
are usually amelanotic lesions.
Most desmoplastic melanomas are variants
of lentigo maligna melanoma.
| Microscopic features: Poorly demarcated, infiltrating intradermal tumours often with
sparse cellularity.
The tumour consists of elongated spindle-shaped
(fibroblast like) cells surrounded by mature collagen bundles.
A few
scattered cells display hyperchromatic, atypical nuclei. Occasional mutinucleate cells may be present.
The tumour displays haphazard, fascicular
or storiform growth pattern.
The stromal component varies in different
tumours.
In spindle cell melanoma there is less desmoplasia.
In desmoplastic melanoma there
are scattered collection of lymphocytes and plasma cells.
It
is often difficult to find melanin in usual
Hematoxylin and
Eosin sections.
Small foci of neural transformation
and neurotropism may be present.
The
presence of neurotropism correlates with a tendency to local recurrence.
Mitotic figures
are usually present.
Desmoplastic melanoma is often
associated with a lentigo maligna epidermal component overlying or
towards one edge of the lesion.
The tumour infiltrates deep and it may be difficult to
estimate the full extent of the tumour.
Immunohistochemistry:
The tumour cells are positive for S100 protein
and neuron specific enolase in about 95% of cases.
HMB45 is usually negative in desmoplastic melanoma.
In spindle cell melanoma about 50% of cases show some HMB45 positivity
(these cases have aggressive behaviour)
Melan A is negative in
desmoplastic melanoma. It has been reported that some cases of metastatic
desmoplastic melanoma are CD34 positive.
Actin is also expressed in some
cases.
Occasionally, the spindle cells of desmoplastic melanoma can be negative
for S100 protein , making distinction from other spindle cell lesions difficult.
|
Differential
Diagnosis:
Desmoplastic melanoma should be distinguished from other spindle cell
lesions such as sclerosing melanocytic nevi,
nodular fasciitis, atypical fibroxanthoma,
dermatofibrosarcoma protruberance
and spindle
cell squamous carcinoma and scar tissue.
Unlike immature scar tissue, in desmoplastic melanoma there is neurotropism, epidermal proliferation of melanocytes, and S100
protein and/ or HMB45 positivity.
(Histologic
differentiation of desmoplastic melanoma from cicatrices.
Am J Dermatopathol.
1998;20(2):128-34)
The sclerotic/desmoplastic and
hypopigmented blue naevi are uniformly positive for Melan-A, while
desmoplastic melanoma is negative in the spindle cell compartment.
The nuclei in desmoplastic melanoma have a haphazard pattern and in scar
tissue the nuclei have a parallel arrangement.
Spitzoid melanoma (cells are more plump) should also be excluded from
spindle cell melanoma (cells are longer and thinner, less aggressive
clinical behaviour).
Neurotropic Melanoma:
Neurotropic melanoma is a rare variant
of cutaneous melanoma.
The tumour has high incidence of local
recurrence and low rate of distant metastases
The neurotropic melanoma is characterized by spindle shaped cells showing
neuroma-like pattern.
These tumour cells infiltrate around nerve bundles
in the deep dermis and subcutaneous tissue. Hence the lesion is called neurotropic
melanoma.
Often a combined desmoplastic and neurotropic
patterns are present.
Differential diagnosis
: Neural and melanocytic lesions (desmoplastic melanocytic nevus ,
neurofibroma
and
malignant schwannoma).
| Diagnostic clues:
- Search for
lentiginous and junctional components in a spindle cell lesion of
actinically damaged skin.
- Asymmetrical
lesion.
- A greater degree of
atypia in the deep dermal and subcutaneous components.
- Single files of
atypical spindle cells among sclerotic collagen bundles.
- The lymphoid reaction
at the advancing edge of the lesion.
- Neurotropic growth.
Invasion of deep vascular channels
|
|